
Blood Pressure
last authored: Dec 2012, Laura Clademenos
last reviewed:
Introduction
Blood pressure is the force exerted by blood within blood vessels as a
result of the pumping action of the heart.
An adequate blood pressure is necessary for blood to travel from the
heart around the body. A blood pressure that is too low (hypotension)
can lead to inadequate blood flow, or hypoperfusion, of critical
organs. A blood pressure that is too high (hypertension) can, over
time, have detrimental health effects on organs such as the heart
(myocardial infarction), the brain (stroke, hemorrhage), and kidneys
(renal failure).
Blood pressure values are measured in mmHg (millimeters of mercury,
atomic symbol Hg). A blood pressure of 100 mmHg, for example, means
that the force generated would push a column of mercury, against
gravity, 100 mm vertically. Blood pressure readings are presented as a fraction. The systolic blood
pressure, the numerator, is defined as the peak pressure during the
cardiac cycle, i.e. when the ventricles are contracting. The diastolic
blood pressure, the denominator, is the pressure when the ventricles
are relaxed. For example, a blood pressure of 120/80 represents a
systolic pressure of 120 mmHg and a diastolic pressure of 80 mm Hg.
If the vascular system were not distensible, each cardiac cycle would
send blood through arteries only during systole, during ventricular
contraction. However, since vessels have elastic properties, they
stretch during systole and gradually return to their resting size
during diastole. This reduces the pulse pressure (the difference
between systolic and diastolic pressure) and allows for more constant
flow through capillaries.
Arteries are not very compliant, seeing only modest increases in volume
following increases in pressure. This gives them the name resistance
vessels. Veins are able to accommodate a larger volume of blood than
arteries. They have a higher compliance and thinner walls, allowing
them to function as capacitance vessels (Andreoli et al, 2010).
Vessel compliance can decrease temporarily with smooth muscle
contraction, and also with age. Hardened arteries will experience
increased systolic pressure and decreased diastolic pressure, leading
to decreased capillary flow.
Physiologically, blood pressure is related to the product of the
cardiac output and total peripheral resistance (BP = CO x TPR).
● Cardiac output is the amount
of blood leaving the heart with each contraction
● Total peripheral resistance
is sum of the resistance of all the blood vessels in the systemic
circulation. Resistance relates to length, radius and number of blood
vessels, as well as the viscosity of blood.
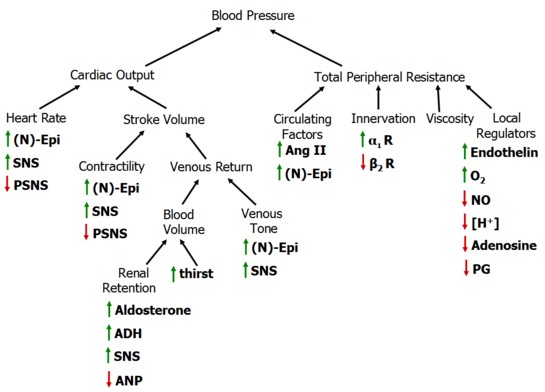
Changes to CO and TPR, and therefore BP, are regulated by the autonomic
nervous system, which consists of the sympathetic and parasympathetic
nervous systems.. Increased activity of the sympathetic nervous system
(SNS) results in increased cardiac output contraction of arterioles,
which increases systemic resistance.
Regulation of cardiac output is described in detail here; the following
information focuses on peripheral resistance.
The Physics of Blood Pressure
Pouiseuille’s law explains the relationship between pressure and flow.
When blood flows through a vessel, the resistance (R) to that flow is
determined by the characteristics of the blood and the vessel,
including viscosity, length (L), viscosity (n) and radius (r). R ∝ Ln/r4
As fluid viscosity or tube length increases, resistance to blood flow
increases proportionately. However, these tend to be constant in human
physiology. This leaves vessel radius to allow adjustment of peripheral
resistance, and as the equation describes, a change in radius has an
leads to a large change in resistance. This variation principally
occurs in the arterioles, where small changes to arteriolar radius can
exert large effects in resistance and therefore flow to an organ.
Arteriolar resistance is controlled by three major mechanisms: local
regulation, sympathetic innervation, and circulating hormonal factors.
Local Regulation
Blood pressure is constant throughout the body, and regional blood flow is adjusted to provide more or less blood to certain tissues to meet functional needs. Arteriolar smooth muscle senses changes in blood flow direction through stretch receptors. This automatic regulation leads to changes in vessel radius directly. Local metabolic conditions also impact vessel radius, as increased cellular activity suggests increased demand for blood flow. Decreased oxygen, increased CO2, increased nitric oxide, decreased pH, increased [K+], or increased adenosine all represent increased metabolic activity and lead to vasodilation.
Inflammation also involves vasodilation in an effort to combat
pathogens and speed healing, mediated by bradykinin and histamine.
Conversely, serotonin is released by platelets to lead to
vasoconstriction during tissue damage.
return to top
Sympathetic Innervation
main article: sympathetic nervous system
Blood pressure is heavily influenced by neurally mediated baroreceptors
- stretch-sensitive nerve endings that transmit afferent impulses to
the central nervous system. High pressure baroreceptors are
found in the carotid artery (the carotid sinus) and the wall of the
aorta (aortic arch). Low pressure baroreceptors are found in the right
atria and pulmonary arteries.
In response to baroreceptor activation, a reflex sends signals back to
the body through the SNS and PSNS efferents. Decreases in blood
pressure, and therefore stretch, prompt signals to transmit to control
centres in the medulla. Activation of the SNS leads to efferent
neuronal signals to the heart and vasculature, resulting in increased
heart rate and contractility (cardiac output) and total peripheral
resistance. These signals are mediated by the neurotransmitter
nor-epinephrine (nor-adrenaline). Sympathetic innervation of the
adrenal gland leads to release of the related sympathetic hormone
epinephrine (adrenaline). Together, these raise blood pressure.
Sympathetic (SNS) activity increases:
- heart rate and contractility
- arteriolar vasoconstriction (increased total peripheral resistance)
- venous vasoconstriction and increased venous return
- sodium and water retention in kidney
- renin release (see below)
- ADH release (see below)
Conversely, when blood pressure (mean arterial pressure) rises, stretch
receptors sense the rise in arterial pressure and increase the firing
rate from the baroreceptors. This information is sent to the medulla in
the brain stem to cause a number of changes: efferent SNS outflow is
inhibited while the PSNS efferent response is increased.
Atrial natriuretic peptide (ANP) is released by the muscle fibres of
the cardiac atria. It is released in response to atrial stretch, which
can occur with increased blood volume. ANP acts on the kidneys to
decrease Na+ reabsorption by the collecting ducts and increase the
glomerular filtration rate. This allows the kidney to excrete more salt
and water, thereby acting to compensate for the excess blood volume.
Compared to other regulators of blood pressure, ANP exerts a relatively
minor effect (Guyton and Hall, 2006).
return to top
Circulating Hormonal Factors
main article: RAAS system
The kidney plays an important role in volume regulation and therefore
blood pressure control. Firstly, it controls how much fluid is excreted
or retained, directly impacting total blood volume. Additionally,
through the activation of the renin-angiotensin-aldosterone system
(RAAS), it has the potential to change the resistance in the arterioles
of the kidney and cause the release of powerful chemical mediators to
change peripheral vascular resistance.
The juxtaglomerular apparatus is found on the afferent and efferent
arterioles of the glomerulus. It is made up of 3 different types of
cells: juxtaglomerular, macula densa, and mesangial. The
juxtaglomerular cells are smooth muscle cells found on the afferent
arteriole, and their function is to secrete renin. Macula
densa cells detect changes in sodium concentrations and send out local
vasoconstrictors to decrease or increase blood flow to the kidney. The
function of mesangial cells is not well understood, but they are
thought to influence the RAAS in coordination with the 2 other types of
cells.
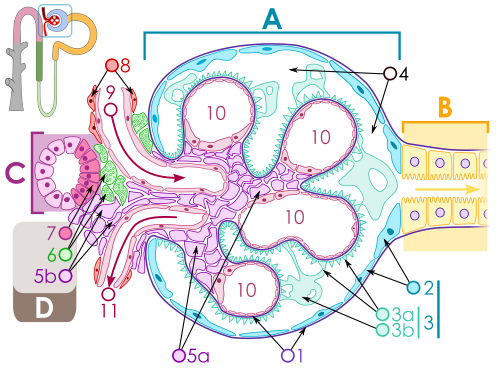
Renal Corpuscle, used with permission by Micha? Komorniczak
Renin is the enzyme released by the kidneys in response to these
signals. By activating the RAAS, its effects include arteriolar
vasoconstriction (increased resistance) and decreased excretion of salt
and water by the kidneys (increased volume). These act to raise blood
pressure.
Renin converts angiotensinogen into angiotensin I (AI). The angiotensin
converting enzyme (ACE) then converts AI into angiotensin II (AII). AII
is a potent vasoconstrictor, acting on arterioles both systemically and
locally at the level of the kidney. AII also causes the release of ADH
and aldosterone.
Aldosterone is secreted from the adrenal glands and acts to increase
the reabsorption of salt from the Loop of Henle. Since water follows
salt, this results in water retention as well. Aldosterone has a longer
term impact on blood pressure control.
Anti-diuretic hormone (ADH), or vasopressin, is secreted from the
posterior pituitary. It works on the kidney to increase the
permeability of the collecting ducts, mediating its effect by inserting
aquaporins into the ducts which helps increase the reabsorption of
water.
return to top
Summary
Blood pressure control is of central importance to physiologic balance,
and there are numerous mechanisms at the local tissue level, within the
central nervous system, and hormonally. These act in concert and at
different speeds to respond to changes in blood pressure, maintaining
healthy perfusion to vital and peripheral tissues.
return to top
Resources and References
1) Guyton, A. C., Hall J. E. (2006). Textbook of Medical Physiology
(11th ed.). Philadelphia, PA: Elsevier Saunders.
2) Andreoli T. E., Benjamin I. J., Griggs R. C., Wing E. J. (2010).
Andreoli and Carpenter’s Cecil Essentials of Medicine (8th ed.).
Philadelphia, PA: Elsevier Saunders.
3) Bickley L. S., Szilagyi P. G. (2009). Bates’ Guide to Physical
Examination and History Taking (10th ed.). Philadelphia, PA: Wolters
Kluwer Health - Lippincott Williams and Wilkins.
