
Heart Rate
last authored:
last reviewed:
Introduction
Normal resting heart rate for adults ranges from 60-100 bpm to maintain adequate cardiac output. Heart rate increases during exercise or stress, largely mediated by neural and hormonal control.
Cardiac contractility is coordinated by pacemakers and the conduction system of the heart, and electrically occurs via cardiac action potentials.
Pacemakers and Conduction System of the Heart
The coordinated cardiac cycle is due to the conduction system distributing impulses throughout the heart.
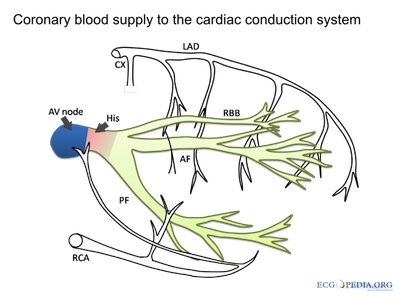
courtesy of ECGpedia.org
Located in the posterior wall of the superior vena cava, the Sinoatrial (SA) Node is the physiologic pacemaker of the heart, with an intrinisic firing rate of 60-100 impulses/min. It is a small mass of cells which emit regular electrical impulses across both atria, like ripples in a pond. Intercalated discs and gaps junctions among cardiomyocytes allow direct flow from cell to cell. SA nodal rate can be influenced by neural or hormonal signaling.
Internodal pathways lead across the atrium to the AV Node, located between the electrically resistant AV valves. It is the the only spot where current can pass to the ventricles. Fibres here are smaller in diameter, and the impulse is thereby slowed to allow time for the atria to contract and empty before ventricular systole. If the SA node or atria are not functioning properly, the AV node can act as a pacemaker, firing at 40-60 impulses/min.
The Bundle of His (AV bundle) leaves the AV Node and splits into the right and left bundle branches, which innervate the ventricles via Purkinje Fibres. Purkinje fibres spread along the endocardium, and the lower part of the ventricules contract before the upper parts. In the absence of both nodal pacemakers, the Bundle of His and Purkinje Fibres can fire at 15-40 impulses/min. This rate is unable to sustain life for long.
Conduction Velocities in the Heart
- SA, AV nodes - 0.05 m/s
- atria, ventricles, bundle branches - 1 m/s
- Purkinje fibres - 4 m/s
Cardiac Action Potentials
The maximum negative voltage of pacemaker cells is about -60 mV, maintaining fast sodium channels in their inactive state.
Pacemaker cells have a spontaneous tendency to depolarization, or automaticity, mediated by the pacemaker (aka 'funny') current If. This is thought to be predominantly via sodium influx though channels which open during repolarization Calcium and potassium also appear to flow.
The pacemaker action potential is slower and lower than that of cardiomyocytes, as it depends solely on calcium influx and not sodium.
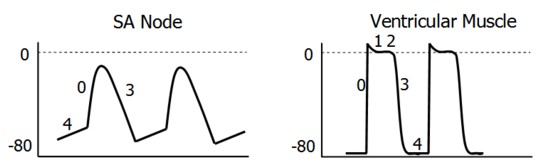
The SA Node and AV node have similar electrical profiles, as do atrial and ventricular muscle and the Purkinje Fibres.
|
|
Differences in pacemaker rate depend on rate of If, maximum negative diasolic potential, and threshold potential. The cell group with the fastest intrinsic rhythm prevents all other automaticity using overdrive suppression. This is due to hyperpolarization which occurs when a cell is forced to fire faster than its pacemaker rate. Molecularly, increased sodium influx requires faster pumping out, resulting in greater intracellular potassium (via the Na/K pump).
The SA node normally initiates the heart beat. Electrical impulses spread through the surrounding atrial muscle through gap junctions, reacing the AV node.
Fibrous tissue surrounds the tricuspid and mitral valves, preventing signals from traveling between the atria and ventricles.
There is a delay of about 0.1 sec at the AV node due to permament inactivation of Na channels in these cells. This allows the atria time to empty, as well as regulates ventricular stimulation during times of abnormal atrial rhythms.
The bundle of His and Purkinje cells, with their very high concentration of sodium channels, rapidly conduct depolarization signals from the AV node across the ventricles.
Neural and Hormonal Control of Heart Rate
Regulation of cardiac output occurs in the medulla, receiving signals from the brain and from baroreceptors.
Heart rate is largely controlled by two opposing forces - The sympathetic system includes norepinephrine released from sympathetic nerves and epinephrine released by the adrenal medulla. Both work on β-1 adrenergic receptors. The parasympathetic system works through acetylcholine.
Sympathetic stimulation increases the slope of pacemaker potential, reducing the time required to reach threshold. Parasympathetic stimulation both decreases the slope and causes the membrane potential to be more negative.
(Nor)ephinephrine increases:
- Conduction velocity of the SA and AV nodes
- increases IFchannel opening - Pacemaker rates of the SA and AV nodes and Purkinje Fibres
- increases ICa2+ channel opening (decreasing firing threshold) - Contraction strength of the atria and ventricles
Acetylcholine decreases:
- Conduction velocity of the SA and AV nodes
- decreases IF (check) - Pacemaker rates of the SA and AV nodes and Purkinje Fibres
- hyperpolarizing the cells via increased K+ permeability
- decreases ICa2+ (and therefore icreases firing threshold) - contraction strength in the atria but very little in the ventricles
