
Menstrual Cycle
last authored: April 2012, David LaPierre
last reviewed:
Introduction
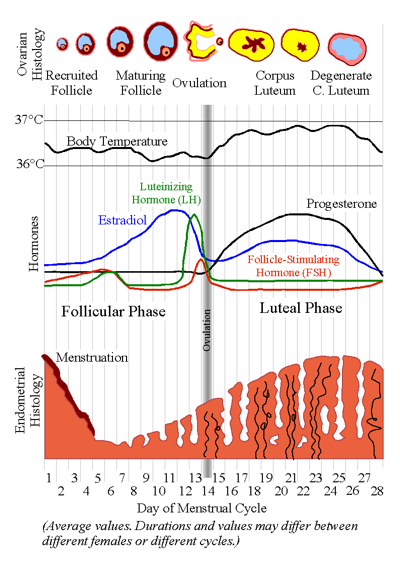
Menstruation normally occurs during cycles of 22-35 days, with menstrual discharge lasting 1-8 days. The cycle is counted from day 1 of menstrual flow until day 1 of the next period.
Menstruation is the periodic loss of uterine lining, or endometrium, including cellular remains, blood, and tissue fluid. The quantity of fluid can vary widely, and the mean blood lost during menstruation is 30 ml, with a range of 10-80 ml.
Some women who have heavy periods are not, in fact, at risk of blood loss anemia.
from Chris73, Wikipedia user
A woman is born with approximately 200,000 eggs, in her ovaries, surrounded by theca lutein cells.
The HPO Axis
The hypothalamus-pituitary-ovary (HPO) axis coordinates the menstral cycle. The development and release of these eggs is under control of two main pituitary hormones - luteneizing hormone (LH) and follicular stimulating hormone (FSH) - which are in turn under control of the hypothalamic hormone gonadotropin-releasing hormone (GnRH), as well as estrogen.
GnRH is released starting with puberty from the hypothalamus in a pulsatile fashion of approximately 90 minutes. and acts on the anterior pituitary to release LH and FSH.
Follicular phase
With each mentstrual cycle, 3-30 ovarian follicles are stimulated by LH and FSH, with one or more of these follicles rapidly growing and being released from the ovarian wall.
Follicular Stimulating Hormone (FSH) is a key reproductive hormone. It acts on primary follicles by binding to granulosa cells and acting to increase fluid secretion into the follicular cavities. This causes them to grow rapidly. Granulosa cells also respond by secreting increasing levels of estradiol into the circulation.
Acting systemically, estradiol at first causes a decrease in pituitary hormones. However, with increasing estrogen, a large LH and smaller FSH surge occurs. This pulse causes ovulation - release of the ovum from the largest follicle.
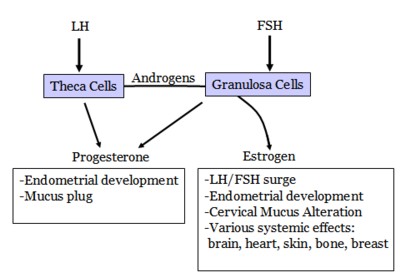
FSH, together with LH, prmotes estrogen production by the ovary. It also induces egg development.
In males, FSH induces sperm development.
LH promotes ovulation and stimulates progesterone following egg release. Together with FSH, it stimulates secretion of estrogen from the ovary. In males, LH stimulates production of testosterone in the testes.
LH is essentially absent until puberty. It is regulated by GnRH release from the hypothalamus.
Secretory/Luteal Phase
During the secretory phase of the menstrual cycle, which is of fixed duration, the endometrium prepares to receive a fertilized ovum by becoming thicker and more vascularized. The endometrial glands become engored with secretions.
These changes are driven by progesterone from the corpus luteum, and peak approximately one week after ovulation.
Predecidualization also occurs, with stromal cells transforming into rounded decidual cells and spreading across the endometrial surface to form the zona compacta. With fertilization, decidualization is sustained and extended in preparation for implantation of the zygote.
In the absence of fertilization, progesterone levels decrease as the corpus luteum dries up, and the thickened endometrium begins to fall away. This is menstruation.
- ovulation
- endometrial cycle
- cervical cycle
- vaginal cycle
Ovulation
Oocytes are arrested in prophase of the first meiotic division.
Following the LH surge, the first meiotic division occurs, resulting in formation of a polar body and a secondary oocyte with a haploid number of duplicated chromosomes.
The second meiotic division is begun but arrests in preparation for fertilization.
Once the ovum has been released, the follicle collapses and becomes the corpus luteum. Namned for its colour yellow, theca granulosa cells become theca lutein cells and secrete progesterone and estrogen.
Progesterone reaches a plateau 4 days post-ovulation, and progressively rises if a fertilized ovum implants into the endometrium. One of the main signals for this is hCG. However, in the absence of implantation, the corpus luteum degenerates and progsterone and estradiol levels fall. This leads menstruation and to renewed secretion of FSH to begin the cycle again.
Ovulation animation, use permitted by Andrew R. La Barbera, PhD, University of Cincinnati, 2007
Endometrial Cycle
The Follicular Phase Begins with Menstruation
The superficial and middle layers of endometrium are shed during menstruation, while the deep layer remains. Shedding occurs in an irregular pattern, with some areas undergoing repair while others slough off. Endometrial vasculature is sealed by hemostasis and vasoconstriction.
Shed tissue coagulates in the uterine cavity but is usually liquified by fibrinolysis, or enzymatic activity. Fluid and tissue is discharged through the cervix by uterine contractions, mediated by prostaglandins. If increased blood loss occurs, fibrinolytic capacity may be overwhelmed and clots can be discharged.
Once the endometrium is shed, a rapid period of development begins. Stromal cells, present in the connective tissue undergo metaplasia (a change in cell type) to form the endometrial surface, and epithelium forms numerous glands. Repair is complete within 3 days of the cessation of menstruation.
During the early proliferative phase, lasting from days 3-7, glands are straight and narrow. Proliferation increases after one week, with epithelial hypertrophy and transition from cuboidal to columnar. Stromal fibroblasts become spindle-shaped.
Arteries leave the myometrium at right angles and supply the endometrium, where they become spiralled. As the endometrium continues to grow, the arteries uncoil to continue providing vascular supply.
Luteal Phase
The luteal phase marks ovulation. Glandular epithelial cells develop secretory vacuoles of increasing number, causing glands to become tortuous. Vacuoles, which are initially subnuclear but then move more apically (towards the surface), are filled with mucus and other molecules to prepare the endometrium for implantation. Peak release occurs at day 6 post-ovulation.
In the absence of pregnancy, estrogen and progesterone levels fall, increasing endometrial levels of arachidonic acid and endoperoxidases. Stromal cells then begin synthesis of prostaglandins PGF2a and PGE2, along with prostacyclin. PGF2a and PGE2 cause vasoconstriction and uterine contraction, while prostacyclin opposes these actions by causing muscle relaxation and inhibiting platelet aggregation. A relative increase in PGF2a causes arteriolar vasoconstriction and reduced capillary blood flow, shunting fluid from the endometrium into the capillaries and decreasing tissue thickness. Hypoxia and ischemic necrosis also occurs, marking the beginning of menstruation.
Cervical Cycle
During the follicular phase, the cervical canal begins secreting thick mucus from glands to form crosslinked mesh. Prior to ovulation, the surge in estrogen leads to action of metalloproteinases that thin the cervical mucus and lead to stranding and channel formation through which sperm can travel. Progesterone, released from the corpus luteum, again causes the cervix to be blocked by thick mucus, reducing passage to and from the uterus.
Vaginal Cycle
The vaginal epithelium responds to the ratio of estrogen and progesterone. During the follicular phase, both superficial and large intermediate cells are seen, while prior to ovulation, greater numbers of superficial cells, along with leukocytes are present.
Following ovulation, increased levels of progesterone leads to large numbers of intermediate cells and leukocytes.
Hormonal Imbalance
androgen excess
estrogen excess
|
progesterone excess
|
estrogen deficiency
|
progesterone deficiency
|
Estrogen
Estrogen initiates female pubertal development, including breat development, widening of the pelvis, and distribution of body fat.
Together with progesterone, estrogen regulates the menstrual cycle.
plasma estradiol levels during the menstrual cycle
phase
|
plasma levels (pmol/L)
|
FSH, released from the anterior pituitary, acts on granulosa cells in the ovary, inducing their production of estrogen.
