
Respiratory Control
last authored:
last reviewed:
Introduction
Respiratory control determines breathing rate and quality to facilitate adequate oxygenation rapid homeostatic balance of pH. The drive to breathe comes from the need to remove CO2, not to inhale oxygen.
The brainstem processes information from various sensors, (as below) and sends signals via the sympathetic nervous system to control the size of airways, glands, and blood vessels.
Sensors
Central chemoreceptors in the medulla detect changes in pH, PaCO2, and PaO2.
Peripheral chemoreceptors in the carotid body are most sensitive to PaO2
Mechanoreceptors in the lung receptors respond to stretch. J receptors, located in the juxtacapillary regions of the lung periphery, respond to vascular engorgement. Irritant receptors respond to physical and chemical stimuli. Lung receptors signal via the vagus nerve.
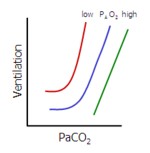 Normally, PaCO2 is the main stimulus for breathing, acting on the central receptor and carotid and aortic chemoreceptors. Hockey stick curves demonstrate how small increases in PaCO2 can have a dramatic effect on ventilation at various PaO2.
Normally, PaCO2 is the main stimulus for breathing, acting on the central receptor and carotid and aortic chemoreceptors. Hockey stick curves demonstrate how small increases in PaCO2 can have a dramatic effect on ventilation at various PaO2.
PaO2 normally plays little role in the stimulus to breathe until it drops very low; the increase in ventilation becomes steep when PaO2 drops below 40 mm Hg.
During exercise, stretch receptors in joints become activated and induce the lungs to breathe.
Having COPD reduces the PaCO2= mediated stimulus to breathe, giving them the name carbond dioxide retainers. Administering oxygen can eliminate the drive to breathe, killing them.
Neuronal control of respiration stems from the DRG and VRG nuclei in the medullary reticular formation, with imput from the pons. The cerebral cortex modifies breathing by conscious control.
