
Pelvic Exam
last authored: July 2011, David LaPierre
last reviewed: Nov 2011, Joseph Ana
Introduction
The female physical exam may be a source of anxiety or discomfort for women, and should be approached carefully, with maturity, sensitvity, and confidence.
There should always be a chaperone when a patient of opposite sex is to be examined intimately. The chaperone must be of the same sex as the patient to be so examined, and does not need to be a nurse. The important thing is that a third party of the same sex as the patient is in the room and the patient is aware of the fact. The chaperone may be outside the screen but in the room.
An exam should begin with discussion of a patient's concerns. The patient may find it helpful to learn more about her body, and the woman's sentiments may be explored beforehand. Obtain a ‘ written informed consent’ or at least document a ‘ verbal informed consent’ from the patient.
Allow the woman to disrobe in privacy, and provide her with a sheet to cover herself with.
External Exam
Don gloves.
Begin with inspection of external genitalia. Note:
- vulva: atrophy, cough stress test, valsava prolapse
- perineum
- scars
- discharge; take swabs for microscopy, culture & sensitivity if discharge appears abnormal.
Speculum Exam
Ensure proper lighting, with a headlamp, a wall/floor mounted light, or with help from an assistant. Have all equipment ready before positioning the patient, and test the speculum for proper function and adequate tightening of the bolt.
Warm the speculum with water. Many clinicians prefer a small amount of water-soluble lubricant on the outer bottom blade, though others will not use this if a pap test will be done.
Provide information about each step before proceeding. Say, "You're going to feel me touch you now". Begin with a hand on the inner thigh before spreading the labia with one hand.
Insert the speculum, examining the vagina as the speculum is advanced. Many clinicians begin with the blades aligned vertically. Open the blades gradually as you proceed smoothly and gently, with pressure aimed downwards to avoid causing pain or damage to the urethra.
Bring the cervix into view. This can be challenging in some cases, made more difficult by obesity, multiparity, or position of the uterus. Repeated practice is required to become skilled at this. If you are struggling, a bimanual exam (see below) can be helpful to spatially locate the cervix. Once the cervix is visualized, lock the speculum into place.
Visualize the cervix for abnormalities. A variety of images of the cervix are provided here for reference:
- Your Beautiful Cervix (a website of women photographing their own cervix)
Depending on the circumstance, acetic acid application, a pap test, or swabs may be carried out. If you are going to do pap smear, ensure materials (ie slides, preservative, etc) are ready before you start the examination. Warn women that these may be a bit uncomfortable.
When finished, loosen the speculum and close the blades as you withdraw, being careful not to pinch the vaginal walls as the speculum closes. Again, many clinicians rotate the speculum to vertical alignment as they withdraw.
Bimanual Exam
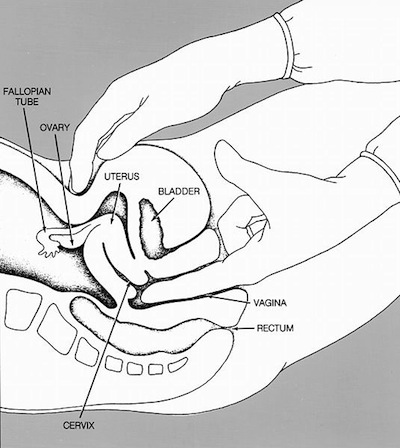
bimanual exam; courtesy of National Cancer Institute
The bimanual exam typically follows the speculum exam. Again, describe what you are doing to the woman before you do it.
Insert two fingers into the vagina after applying a water-based lubricant to the fingers. Place the other hand on the abdomen to sandwich the uterus and adnexa between the two hands.
Palpation will reveal the consistency, length, and dilation of the cervix. Cervical motion tenderness may suggest inflammation, such as can occur with infection.
Uterus size and ante/retroflexion should also be apparent. Uterine size is normally the size of an orange.
Adnexal masses may be felt on either side of the uterus, if present. Ovaries are approx 2x2cm, may be palpable, and can be slightly tender. This is normal.
In pregnancy, a bimanual exam can reveal the presenting part.
Rectovaginal and rectal examinations can be done to provide further information, as required, but should be carefully explained.
At the end of the exam, dry the perineum with gauze or paper towel before removing gloves.
Resources and References
University of Florida - clinical skills teaching resources
Merck Manual - approach to the gynecologic patient
Brookside Associates - pelvic exam video
