
Endometriosis and Adenomyosis
last authored: Aug 2010, Kim Colangelo
last reviewed:
Introduction
Endometriosis is when endometrial tissue, normally found lining the uterus, begins growing outside of the endometrial cavity. It most commonly affects women in their 20ís and 30ís.
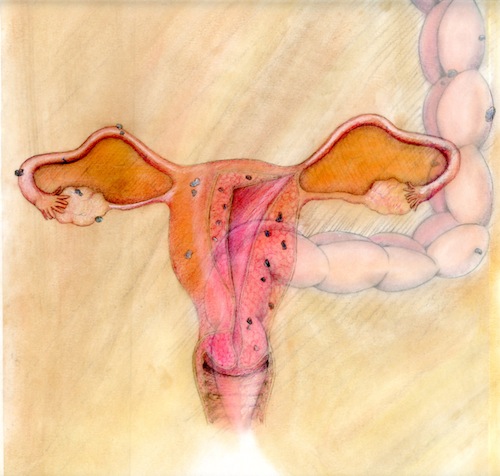
endometriosis and adenomyosis; artwork by Jillian Claeys
Endometriosis can cause a number of significant symptoms. However, women can have evidence of endometriosis and no symptoms, and they can have symptoms that seem to be caused by endometriosis but do not resolve when it is treated.
Adenomyosis, on the other hand, is when the endometrial layer extends into the myometrium. Adenomyosis is seen in an older age group with onset typically in the 40’s and 50’s.
Both endometrial glands and stroma must be present for a histological diagnosis to be made of either endometriosis or adenomyosis.
The Case of Ms Ruth R.
Ruth R is a 35yo G0P0 female who presents to the nurse practitioner at her local womenís health clinic for her annual sexual health check up. She reports 4 months of suprapubic pain and painful intercourse. She has no medical conditions. The pelvic exam is normal and basic bloodwork and cultures have come back negative as well as the routine pregnancy test.
- What systems could be involved here?
- What imaging could help you in making a diagnosis?
Causes and Risk Factors
Risk factors include:
- family history (7-10x increaed risk with 1st degree relative)
- obstruction of genital tract
- age >25 years
- nulliparity
Pathophysiology
The most common place for the endometrial tissue to appear is in the ovaries, also known as an endometrioma. Other places it commonly appears are on the broad ligament, the cul-de-sac, the colon and appendix.
Immunology is thought to make a particular woman more susceptible to endometriosis.
There are several theories for the cause of endometriosis:
Retrograde menstruation (Sampson theory): causes endometrial cells to flow through the fallopian tubes and into the peritoneal cavity
Lymphatic and vascular spread: which would explain how endometrial tissue can be found in remote sites such as the lung
Coelomic metaplasia: Peritoneal epithelium transform into endometrial tissue due to an unknown stimuli, this would explain how endometriosis can occur in women who have had a hysterectomy and are not taking and estrogen supplements Mullerian remnants differentiate into endometrial tissues due to an unknown precipitant.
Signs and Symptoms
- history
- physical exam
History
Because the endometrial tissue undergoes menstrual cycle changes regardless of where it is located, the symptoms related to endometriosis are often cyclical where they worsen right before menses and continue until just after menses.
Common symptoms for endometriosis and adenomyosis:
- Dysmenorrhea (menstrual pain) or menorrhagia
- Deep dyspareunia
- Sacral backache during menses
- Vaginal bleeding other than during menses
- Infertility
- Bladder symptoms – urinary frequency, dysuria, hematuria
- Bowel symptoms – diarrhea and/or constipation, hematochezia
In any chronic pain condition it is important to take a thorough pain history: onset, severity, course, quality, radiation, associated symptoms, precipitants and alleviating factors, patient’s thoughts on the cause of the pain, past investigations, past treatments.
Also take a complete GI, GU, MSK, and psychological history.
Physical Exam
The findings on vaginal exam are most prominent during menstruation:
- A sharp and tender nodule on the uterosacral ligament may be felt
- A firm and fixed adnexal mass could be an endometrioma
- The uterus may be retroverted
For adenomyosis, a bulky uterus may be discovered. It will not be fixed as it can be with endometriosis. It may be symmetrically enlarged or have focal areas of nodularity called adenomyomas. There are no ovarian symptoms for adenomyosis.
Investigations
- lab investigations
- diagnostic imaging and surgical exploration
Lab Investigations
Serum cancer antigen 125 (CA-125) levels may be elevated.
Diagnostic Imaging and Surgical Exploration
Ultrasound may detect an endometrioma or adenomyosis but is unlikely to see endometrial tissue anywhere else. A transvaginal scan is better than a transabdominal for identifying adenomyosis.
An MRI scan is effective at diagnosing adenomyosis with accuracy similar to transvaginal ultrasound.
There are characteristic findings on laparoscopy for endometriosis:
- Lesions seen
- Mulberry spots which are dark blue – brown – black lesions seen, often on the uterosacral ligament or cul-de-sac
- Chocolate cysts on the ovaries (endometrioma) caused by old blood that has hemolyzed
- Powder-burn lesions on the peritoneal surface
Two suspicious areas should be sampled and sent for histology.
There are 4 stages of endometriosis, however what constitutes each stage has changed over the years. The 4 stages are based on the location of the lesions, diameter and depth of lesions, and density of adhesions.
Differential Diagnosis
The differential diagnosis includes:
- Pelvic inflammatory disease
- Pelvic congestion syndrome
- Ovarian: mass (benign or malignant), torsion, hemorrhagic corpus luteum
- Ectopic pregnancy
- Any postmenopausal bleeding is endometrial cancer until proven otherwise
- Dyspareunia – musculoskeletal, bowel, urinary tract, vaginal dryness or irritation
Chronic pelvic pain can also be caused by:
- Bowel– irritable bowel syndrome, inflammatory bowel disease
- Urinary tract– chronic UTI, stones, urethral syndrome
- Musculoskeletal – myofascial pain, pelvic floor spasms, nerve entrapment syndromes, mechanical low back pain, hernias
- Psychological - sexual or psychological abuse, depression, substance abuse, stress
Treatments
NSAIDs can be helpful to control pain and inflammation.
Hormones:
- Continuous oral contraceptive pills – suppress LH and FSH and prevent ovulation
- Medroxyprogesterone injections (Depo-Provera) – similar to OCP
- Danazol – a weak androgen that can be used for a short time period only due to the possibility of osteoporosis development, has numerous side effects such as weight gain, fluid retention, acne, hirsutism, and voice deepening. It inhibits LH and FSH from being released leading to low estrogen and endometrial atrophy
- GnRH agonist (leuprolide, gosarelin) that will negatively feedback to reduce the GnRH secreted also leading to low estrogen, side effects include hot flashes, vaginal dryness, and reduced libido
Surgery
- For adenomyosis a hysterectomy is the only surgical treatment
- For endometriosis:
- Laparoscopic procedure with laser and/or electrocautery to ablate the lesions and lyse the adhesions
- Removal of endometriomas
- Hysterectomy and oophorectomy to prevent cycling
Consequences and Course
Endometriosis has a high recurrence rate, and it is higher with medical therapy then surgical therapy. Chronic pelvic pain from endometriosis can significantly affect a woman's quality of life.
Only surgical treatment has been shown to improve the fertility of patients whose infertility was thought to be due to endometriosis.
Resources and References
- SOGC: Consensus guidelines for the management of chronic pelvic pain. No 164, Aug 2005. http://www.sogc.org/guidelines/public/164E-CPG1-August2005.pdf.
- Picture - http://commons.wikimedia.org/wiki/File:Endometrioma1.jpg Courtesy Wikimedia Commons/Nephron
- Picture - http://commons.wikimedia.org/wiki/File:Endometriosis.jpg. Courtesy Wikimedia Commons/Richie Graham 2005
- Picture - http://commons.wikimedia.org/wiki/File:Perforierte_Endometriosezyste.jpg Courtesy Wikimedia Commons/Gloecknerd 2002)
Topic Development
authors:
reviewers:
