
Parkinson's Disease
last authored: April 2012, David LaPierre
last reviewed:
Introduction
Parkinson Disease (PD) is the second-most common neurodegenerative disorder, following Alzheimer's disease, of the brain. It unfortunately is also one of the most difficult diseases to manage, particularly in the later stages. It progresses from mild functional loss to severe functional automonic, and cognitive impairment.
Key symptoms of PD include tremor, slowness of movement, rigidity, and balance/gait problems.
Parkinsonism is the syndrome describing the movement disorders seen in PD, and can be due to many causes.
PD most commonly begins between ages 45-65. Males are more affected, though all ethnic groups may develop the disease.
The Case of Mrs. Gail E
Mrs. E. is a 78 year-old retired farmer. She comes to her family doctor at the request of her family due to weakness and difficulty moving. As she walks through the door, you immediately notice a shuffling gait and repetititve meovement of the jaw.
- How would you assess for Parkinson's signs and symptoms?
- What tests, if any, do you offer?
- What treatments would you consider for Mrs E?
Causes and Risk Factors
Environmental risk factors for PD have been difficult to identify.
Parkinsonism, however, can be brought on by various medications such as:
- typical and atypical antipsychotics
- antiemetics, eg prochlorperazine, metoclopramide
- calcium channel blockers, eg flunarizine, cinnarizine
- amiodarone
- lithium
- valproic acid
- MPTP is a synthetic byproduct of improper (often illegal) opioid production and is cytotoxic for dopaminergic neurons
Genetics appears to clearly be involved in PD, and 10-15% of patients will have a first degree relative with the disease. Many autosomal and recessive genes appear to contribute risk for symptoms.
Pathophysiology
 Parkinson's is characterized by degeneration of dopaminergic neurons in the substantia nigra pars compacta. Neuronal loss is accompanied by depigmentation and gliosis, as well as the formation of intracellular Lewy Bodies.
Parkinson's is characterized by degeneration of dopaminergic neurons in the substantia nigra pars compacta. Neuronal loss is accompanied by depigmentation and gliosis, as well as the formation of intracellular Lewy Bodies.
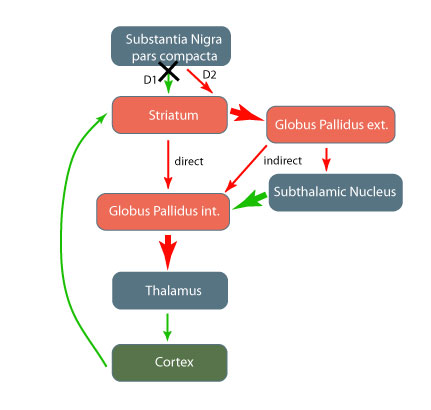
This degeneration leads to increased inhibition of the globus pallidus externa, which in turn causes increased inhibitory output of the globus pallidus interna. This is in part due to increased excitation by the subthalamic nucleus.
The increased inhibition of the thalamus is central to PD's effects. Reduced input to the motor cortex leads to rigidity, bradykinesia, and the other PD symptoms.
Signs and Symptoms
PD can be very difficult to diagnose, as the history is often nonspecific. It should be included in the differential of all seniors who are showing functional decline, and its features should be specifically explored.
- history
- physical exam
History
Symptoms can include:
- motor consequences, as described under 'physical exam'
- depression
- autonomic dysfunction: constipation, incontinence, erectile dysfunction
- loss of olfaction (an early symptom)
- psychotic features: more associated with medications or Lewey Body dementia
Ensure reversible causes are considered.
Physical Exam
TRAP
- tremor
- rigidity
- akesia
- postural instability
Cardinal features of PD include:
Tremor
- typically resting tremor at ~4-8 Hz (cycles/second)
- usually in one upper limb first, then spreading to ipsilateral lower limb
- often disappears with movement, though hand tremor can be brought on while walking
- cranial tremors can affect the tongue, jaw, and chin
- micrography
Bradykinesia - decreased amplitude and velocity of voluntary movement
- may be perceived as weakness, though with normal strength testing
- low volume speech
- shuffling gait
- decreased swallowing and increased drooling
- decreased arm swing
- blephrospasm
- akinesia - impaired initiation of movement
Rigidity
- stiffness can be associated with discomfort
- cogwheel rigidity: recurrent 'catching' when assessing tone of biceps or wrist
- leadpipe rigidity: stiffness present throught range of motion
- masklike face (hypomimia)
Postural disturbances
- stooped posture
- impaired balance
- falls
- gait changes: forward flexion, shuffling (festinating) gait, freezing
- en-bloc turning
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
Lab investigations have a limited role in PD diagnosis.
Diagnostic Imaging
Imaging is of limited value in the diagnosis, though can be helpful to rule out other conditions.
CT can show leukoariosis.
MRI can help rule out other disorders such as multiple sclerosis or tumor
Differential Diagnosis
The differential diagnosis for PD includes:
- essential tremor: generally symmetrical, hand, head, and voice involvement, no rigidity or bradykinesia, large handwriting
- spacticity
- drug-induced parkinsonism
- Parkinsonian syndromes (, vascular)
- Lewy body dementia: hallucinations, falls
- unusual "Parkinson's plus" conditions (progressive supranuclear palsy, multiple systems atrophy)
Treatments
A diagnosis of PD can be made with a two-week trial of levodopa, with videotaping pre- and post. The timed up-and-go (TUG) can easily be done to assess performance.
Non-pharmacotherapies
Rehabilitation, including physiotherapy and occupational therapy, can be very helpful. Exercise should be encouraged for as long as possible. Speech therapy can be provided if dysarthria is present. Dietary advice may be helpful regarding dysphagia and to prevent constipation.
Medications
Drug therapy, which typically act ton increase dopamine levels, should be considered when symptoms interefere with regular function. Options include:
levodopa/carbidopa
- taken up by dopaminergic neurons in the substantia nigra and converted into dopamine; works only as long as dopaminergic neurons remain - perhaps 15 years
- carbidopa does not enter brain; acts to prevent peripheral transformation to dopamine
- rapid onset and offset between doses
- better for patients over 65, given complications that can develop
- can cause dyskinesias, psychotic symptoms, sleep attacks, orthostatic hypotension, GI effects
dopamine receptor agonists: pramipexole, ropinirole, pergolide, bromocriptine
- directly activiate D2 receptors in striatum
- do not require dopaminergic neurons
- less motor symptoms than levodopa, but many others specific to given drugs
Other options include: anticholinergics, (eg benztropine), MAO-B inhibitors, NMDA antagonists such as amantadine, COMT inhibitors.
Atypical neuroleptics are sometimes used for Parkinsonism symptoms.
Surgical procedures
New surgical techniques include:
- pallidotomy
- deep brain stimulation of subthalamic nuclei using electricity to inhibit - this leads decreased globus pallidus signaling
- neural transplantation
Advanced PD
Combination drug therapy is often used
Some problems which do not respond to drugs include:
- hypophonia
- swallowing problems
- balance problems
- freezing episodes
- cognitive impairment
Approximately 5 yrs after levodopa, 50% of pts develop
- on-off fluctuations
Axial motor complications
- dropped head syndromes
Autonomic symptoms
- urine
Consequences and Course
PD is a progressive disease, even with medication therapy. Mortality is over 1.5 that of age-matched patients.
Complications can arise from the disease itself or from the treatments. These can include:
- depression, apathy
- anxiety
- psychosis
- dementia, impulse control
Resources and References
Topic Development
authors:
reviewers:
