Pelvic Inflammatory Disease
last authored: Aug 2010, Kim Colangelo
last reviewed: Dec 2011, Christopher Dainton
Introduction
Pelvic inflammatory disease (PID) is a common condition in females, particularly young women of child bearing age. It is a spectrum of conditions that can range from acute to chronic and involve varying degrees of illness.
PID involves infection by a number of potential pathogens of the upper genital tract, specifically the uterus ands fallopian tubes. However, infection can spread to other structures in the pelvis and can also extend to the intra-abdominal area.
The Case of Rachel T
A 24yo nulliparous female presents to the emergency department with constant left lower quadrant pain of 2 days duration. Upon questioning she believes it started after intercourse with her partner. She is in a monogamous relationship and uses no contraception. Her periods are regular qmonthly of 3-4days duration of moderate flow and her last menses was 14days ago.
Where is she in her menstrual cycle? What happens at this time that could cause her pain? If you could do one thing on physical exam and one lab test what would it be?
Causes and Risk Factors
PID is often polymicrobial:
- Chlamydia trachomatis
- Neisseria gonorrhea
- Natural vaginal flora – E. coli, Staphylococcus, Streptococcus, Enterococcus, Bacteroides, Peptostreptococcus, Haemophilus influenza, Gardnerella vaginalis
- Actinomyces israelii
However, some clinicians define PID as being caused by Chlamydia and/or N. gonorrheae, referring to other infections as pelvic infection.
Risk Factors
- Age <30yo
- the same as for chlamydia and gonorrhea: young age at first intercourse, multiple or new sexual partners, symptomatic partner
- previous episode of PID
- vaginal douching
- intrauterine device (IUD) insertion within first 10 days
- gynecologic procedures (D&C, endometrial biopsy)
Pathophysiology
Not all women with Chlamydia or gonorrhea go on to develop PID; what causes it's development is not known for certain. PID involves two stages, the first being infection with a causative organism. The second stage involves ascent of the organism to the upper repreoductive tract, include:
- menstruation, whereby the cervix is opened
- intercourse, where uterine contractions draw sperm up, bringing pathogens with them
- hormonal change in protective vaginal mucus potentially allowing overgrowth of organisms
The natural vaginal flora has many potentially pathogenic organisms that can overgrow when the normal Lactobacilli flora is disrupted. If it is an anaerobic organism, bacterial vaginosis usually results. Bacterial vaginosis is not an inflammatory condition and is thus separate from PID.
Actinomyces israelii is associated with IUD’s, particularly those that have been in place for a prolonged period of time. This type of PID may present differently, with a pelvic mass and constitutional symptoms being more predominant. Actinomyces can be cultured on a cervical swab of a woman without PID so antibiotic treatment should only be initiated if the woman is symptomatic.
The potential long term complications are result of scarring and adhesions from the inflammatory process in the pelvis. These are described below under consequences and course.
Signs and Symptoms
- history
- physical exam
History
May be asymptomatic
Lower abdominal pain is the most common presenting symptom
- Fever >38.3
- Cervical or vaginal discharge
- Irregular vaginal bleeding
- Dysuria
Chronic PID is associated with constant suprapubic pain, dyspareunia
Physical Exam
Vital signs should be performed to assess for shock.
Abdominal exam:
- tenderness, guarding, rigidity
Pelvic exam
- cervical motion tenderness with/without uterine or adnexal tenderness (classic)
PID is usually a clinical diagnosis and many physicians will initiate treatment based on cervical motion tenderness alone.

Speculum exam revealing PID, courtesy of CDC PHIL
An endometrial biopsy has been used in the past, which shows plasma cell endometritis. This is not currently part of the recommended work up.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
Beta-HCG to assess for pregnancy should be done in any female of child bearing age presenting with abdominal, pelvic, or constitutional symptoms. It is critical to rule out ectopic pregnancy if unilateral pain is present.
A CBC may show leukocytosis.
Speculum exam with cervical culture for Chlamydia and N. gonorrheae and vaginal swab
Gram stain – if it shows gram negative intracellular diplococci, this is highly suggestive of N. gonorrheae
Urine culture to assess for UTI
Diagnostic Imaging
Ultrasound – can be normal, fluid in cul-de-sac (the anterior and posterior areas outside of the uterus where fluid can pool), pelvic or tubo-ovarian abscess, hydrosalpinx (inflammation in the fallopian tube blocks the drainage of fluid leading to enlargement)
Bowel and bladder investigations as necessary to rule out other potential causes:
- abdominal xray/CT
- gallbladder U/S
Differential Diagnosis
PID can be confused with other conditions as well. Those marked with * are potentially emergent conditions not to be missed acutely!
gynecological
|
genitourinary
|
gastrointestinal
|
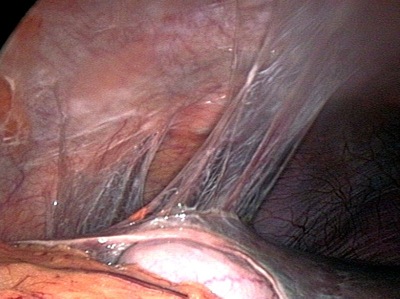
Laparoscopy/laparotomy is rarely needed to make the diagnosis; however, in a very ill patient where the diagnosis is unsure this may be needed to determine the source of infection.
Treatments
The majority of patients with PID will be treated with antibiotics on an outpatient basis. A patient may need to be admitted and given IV antibiotics if they present very unwell, pregnant, with an abscess, an ectopic pregnancy cannot be ruled out, or they are otherwise unable to tolerate oral antibiotics.
A tubo-ovarian abscess is dangerous as it can rupture leading to septic shock. Any patient with this should be admitted to the hospital.
Since Chlamydia and gonorrhea are commonly co-infectious agents they are treated concomitantly with:
- a 3rd generation cephalosporin (gonorrhea) + doxycycline or azithromycin (Chlamydia)
- clindamycin + gentamicin
If the infection is associated with an IUD it may need to be removed, however antibiotics should be started first. There is currently no consensus guideline stating it should be removed however close follow up is recommended.
Screen and treat partners since Chlamydia and gonorrhea are sexually transmitted.
Consequences and Course
Most patients improve within a few days of beginning antibiotic therapy.
Potential complications include:
- disseminated infection, sepsis, and death
- intestinal obstruction
- Fitz-Hugh-Curtis syndrome - perihepatitis where the liver capsule and peritoneal surface are involved. The history reveals RUQ pain that can radiate to the shoulder, potentially confused with cholecystitis
- ectopic pregnancy in subsequent pregnancies due to damage to the fallopian tube
- chronic pelvic pain
- infertility due to damage to the fallopian tube
The mode of transmission of a sexually transmitted infection and how they can protect themselves should be discussed with the patient on follow up.
Resources and References
- Centre for Disease Control. Sexually Transmitted Diseases Treatment Guidelines 2006. http://www.cdc.gov/std/treatment/2006/pid.htm
- Image 1 Centre for Disease Control Public Health Image Library ID#3795, http://phil.cdc.gov/phil/details.asp, courtesy CDC/ Dr. Lourdes Fraw, Jim Pledger
- Image 2 Wikimedia Commons, http://commons.wikimedia.org/wiki/File:Perihepatic_adhesions.jpg, courtesy Wikimedia commons/Gloecknerd 2006.
Topic Development
authors: Kim Colangelo, Aug 2010
editors:
reviewers: