
Placenta Accreta, Increta, and Percreta
last authored: May 2015, Tiffany Klassen
last reviewed: Nov 2015, Dr Neerja Sharma
Introduction
Placenta accreta is used to describe any placental implantation that results in abnormal adherence to the uterine wall (myometrium). It occurs in places within the uterus where the formation of the decidua (outer layer of the uterus) is defective or absent, preventing the normal separation of the placenta after the birth.
The incidence is 1 in 533 pregnancies, up from 1:2510 in the 1980’s and 1:4027 in the 1970’s (ACOG), mainly due to the increase in cesarean rates. There is a high incidence of associated maternal morbidity and mortality, both of which are minimized with prenatal diagnosis.
Causes and Risk Factors
Risk factors that increase the possibility of placenta accreta include:
- maternal age >35
- grand multiparity (parity >6)
- implantation over a previous uterine scar: 0.31% risk of accreta after 1 previous CS, 0.57% after two, 2.13% after three, 2.33% after four and 6.74% after five or more repeat cesareans (Silver, 2006)
The relative risk of placenta accreta in the presence of placenta previa is approximately 1:2000 (Miller, Chollet, and Goodwin, 1997).
The presence of placenta previa and a 1 previous cesarean carries a 25% risk for accreta and more than 40% if more than 1 previous CS (Clark, Koonings, and Phelan, 1985).
Procedures or conditions resulting in changes to uterine tissue:
- uterine curettage
- Asherman’s syndrome
- thermal ablation
- submucous leiomomata (fibroids)
- uterine artery embolization
Pathophysiology
main article: placenta
The placenta is an amazing organ with a fetal and a maternal component. The fetal side develops from the same blastocyst that forms the fetus, and the maternal side develops from the maternal uterine tissue. The ‘decidua’ is the proper name given for the endometrium after implantation, and is rich in blood vessels which provide nutrients to the uterus. This layer is necessary for proper placental formation and cleavage during the third stage of labour.
There are 3 classes of adherent placenta:
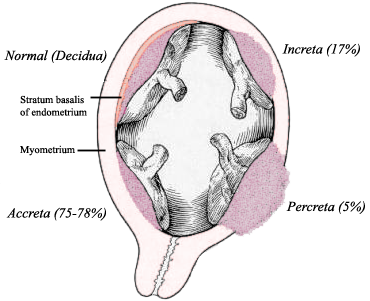
from Gray's Anatomy, public domain
Placenta accreta: occurs when there is either defective decidua or no decidua under the implanted placenta, which normally lies between the placenta and the myometrium, causing the placenta to attach directly to the surface of the uterus.
Placenta increta: occurs when the chorionic villi have invaded into but not through the full thickness of the uterine myometrium.
Placenta percreta: occurs when the villi have invaded the full thickness of the myometrium and grown into, and sometimes even through, the uterine serosa. If the placenta has implanted low and anteriorly, the villi may even grow through the wall of the bladder, resulting in hematuria, and partial or complete uterine rupture in some cases. Intraperitoneal bleeding is common. Associated with single-layer closure of a uterine incision after previous cesarean.
Signs and Symptoms
- history
- physical exam
History
There will be no signs or symptoms antenatally of an abnormally-adherent placenta. There might be possible hematuria if there is percreta into the bladder.
Physical Exam
Most accretas are diagnosed in the third stage of labor when the placenta fails to deliver. If the accreta is complete, the care provider will notice there isn’t any vaginal bleeding and the retention of the placenta will be prolonged, even if the woman is having effective contractions. If the accreta is partial, the patient will continue to bleed, and even though the care provider tries to separate and deliver the placenta, all maneuvers will be unsuccessful.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
During prenatal genetic testing, the patient may have elevated levels of Maternal Serum Alpha-fetoprotein (MSAFP).
Diagnostic Imaging

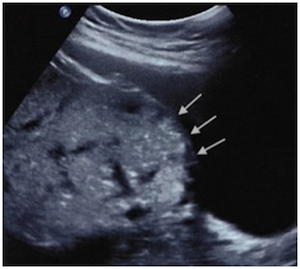
Loss of the normal retroplacental clear space on ultrasonography.
courtesy of Riteau et al, 2014.
Grayscale ultrasound is usually used to diagnose abnormal placentation in the second or third trimester, preferably transvaginal. It has a 77-87% sensitivity and 96-98% specificity.
Signs of abnormal placentation include:
- multiple irregular-shaped venous lakes (vascular spaces) in the placenta
- myometrial thinning under placental implantation site
- loss of the retroplacental “clear space”:
- elevation of tissue beyond uterine serosa/increased vascularity of the uterine serosa-bladder interface or protrusion of the placenta into the bladder.
Ultrasound showing uterine bulging and disruption of
the hyperechogenic uterine/bladder interface
courtesy of Riteau et al
Color Doppler Ultrasound is very helpful in the diagnosis process. Signs of abnormal placentation include dilated vascular channels with diffuse lacunar flow, hypervascularity linking placenta to uterine wall, dilated vessel channels with pulsatile venous flow, and poor vascularity at sites of loss of hypoechoic zone.
If colour Doppler ultrasound is available in a prolonged third stage of labor, an accreta can be diagnosed if there continues to be blood flow from the uterus deep into placenta.
MRI does not add much information diagnostically unless the ultrasound findings are ambiguous or the placenta is posterior and clear ultrasound images are difficult to obtain, or if percreta is suspected.
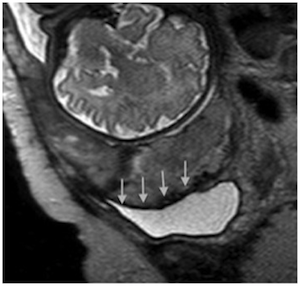
Uterine bulging into the bladder on MRI
courtesy of Riteau et al
Without a prenatal diagnosis, the only way to positively identify placenta accreta is by doing an internal uterine exploration in the third stage of labor in an attempt to manually remove the placenta, and to determine if a normal line of cleavage exists between the maternal surface of the placenta and the uterine wall.
Differential Diagnosis
With prenatal investigation by ultrasound or MRI, there is no differential diagnosis; like stated above, there are no symptoms to be confused with any other disorder. Intrapartum, accreta might be mistaken for a simple retained placenta, but will be properly diagnosed with an attempted manual removal that is not successful.
Treatments
In many parts of the world, prenatal ultrasound is not a typical part of a patient’s care, and antenatal diagnosis of abnormal placental implantation is not made.
Level 1, no prenatal diagnosis
In the case that the woman is bleeding or placenta is retained and you are remote, the best and only option is to try to manually remove the placenta. If the line of cleavage is not easily felt and placenta quickly delivered, abandon the attempt and suspect accreta. Proceed to:
- Follow hemorrhage protocol
- Stabilize patient
- Call for help and transport to the closest hospital
Level 2, no prenatal diagnosis
In the case that the woman is bleeding or placenta is retained, a manual removal can be attempted if the OR is prepped for more aggressive treatment should the placenta not deliver. If the necessary personnel are not available at your hospital, do not attempt a manual removal.
- Follow hemorrhage protocol
- Stabilize patient
- Call for help and transport to the closest tertiary care center.
Level 3 with prenatal diagnosis
If the accreta is diagnosed prenatally, the patient should deliver in a tertiary care centre where expert care providers are available, ideally a team consisting of an obstetrician, paediatrician, gyne oncologist, anesthesiologist, urologist, hematologist, interventional radiologist and other general surgeons. Optimal delivery is a planned preterm (34 weeks gestation) cesarean section with complete hysterectomy with the placenta left in place, as attempts at removing the placenta are associated with high risk of maternal morbidity and mortality.
The health care providers should also study the placenta and uterus after the hysterectomy or placental removal to help diagnose the degree of adherence, as microscopic examination will show chorionic villi in the myometrium.
Keep up the maternal hemoglobin prenatally and keep blood cross-matched.
Conservative management options include:
- leaving the placenta in-situ and giving broad-spectrum antibiotics - has high incidence of suppuration and infection, and eventual hysterectomy
- intrauterine balloon tamponade to compress uterine blood vessels
- selective pelvic embolization
Consequences and Course
With complete accreta, all the cotyledons are attached to the myometrium, and there is no uterine bleeding at all after the delivery of the baby. With partial accreta, only a portion of the surface is attached to the myometrium, greatly increasing the woman’s chances of third stage hemorrhage. When this occurs, the care provider may do all they can to completely detach the placenta, but all efforts will fail, as the woman continues to bleed.
Blood loss averages 3000-5000ml. Up to 90% of patients require a blood transfusion and 40% need more than 10 units of packed red blood cells. This can lead to disseminated intravascular coagulopathy, hysterectomy, injury to adjacent organs, adult respiratory distress syndrome, acute transfusion reaction, electrolyte imbalance, and kidney failure.
Mortality is reported in up to 7% of cases.
In instances where there is excessive pulling on the cord or placenta, uterine inversion or uterine rupture may occur.
If a planned preterm cesarean is pursued, the consequences of a preterm infant must be taken into consideration. Consider corticosteroids.
If the woman’s uterus is able to be saved and she becomes pregnant again, she is at a higher risk of recurrence, uterine rupture, blood transfusions after delivery, and need for hysterectomy.
Resources and References
Clark SL, Koonings PP, Phelan JP. (1985). Placenta praevia / accreta and prior caesarean section. Obstet Gynecol;66:89–92).
Frye, Anne. (2004). Holistic Midwifery, Volume II. Portland, Oregon: Labrys Press.
Varney, Helen. (2003). Varney’s Midwifery, Fourth Edition. Jones & Bartlett Learning.
Oxorn, Harry. (1985). Oxorn-Foote Human Labor and Birth Fifth Edition. McGraw-Hill Medical
Miller DA, Chollet JA, Goodwin TM. (1997). Clinical risk factors for placenta praevia -placenta accreta. Am J Obstet Gynecol;177:210–4.)
Placenta Accreta. (2012) Committee Opinion No 529. The American College of Obstetricians and Gynecologists. Obstet Gynecol. 120: 207-11
Hunt, Jennifer C. (2010). Conservative Management of Placenta Accreta in a Multiparous Woman. Journal of Pregnancy. Volume 2010, Article ID 329618, 5 pages
Riteau et al. 2014. Accuracy of Ultrasonography and Magnetic Resonance Imaging in the Diagnosis of Placenta Accreta. PLoS One. 9(4): e94866.
Mount Sinai Hospital, Areas of Care, Placenta Clinic: Invasive Placenta. Retrieved from: http://www.mountsinai.on.ca/care/placenta-clinic/complications/invasiveplacenta#
Silver RM. (2006). Maternal morbidity associated with multiple repeat cesarean section deliveries. Obstet Gynecol. June; 107(6): 1226-32
Topic Development
authors:
reviewers:
