
Pulmonary Function Tests
last authored:
last reviewed:
Introduction
Pulmonary function testing (PFT) includes spirometry, static lung volumes, and gas exchange (diffusing capacity).
They are used as a screening tool for lung disease, to assess respiratory impairment, monitor disease course or response to treatment, identify baseline lung function for occupation, or to provide preoperative assessment.
Factors influencing normal values include:
- height
- age - increases to peak at age 25
- sex - men larger
- race - Blacks and Asians have ~12% smaller volumes
- posture - little difference between sitting and standing; reduced supine
Indications and Contraindications for PFTs
Commonly evaluated diseases include:
asthma: measure at least q6-12 months for diagnosis, severity, and response to treatment
COPD: use PFTs for early detection, assessment of severity, and monitoring response to therapy
The following people should also be screened:
- smokers >20 pack years
- patients with significant occupational expsure to respiratory irritants
- patients with family history of respiratory distress
Contraindications
PFTs should not be performed if patients have:
- hemoptysis of unknown origin
- pneumothorax
- unstable cardiovascular status
- thoracic, abdominal, or cerebral aeurysms
- suspected TB or other contagious respiratory infections
PFTs are less accurate if there is chest, abdominal, face, or mouth pain; headache, stress incontinence; in children; and with dementia or confusion.
Measures of Lung Function and Volume
- spirometry
- lung volumes
Spirometry
FVC = forced vital capacity = volume exhaled after maximal inspiration through to maximal expiration
FEV1 = forced expiratory volume in 1 sec
FEV1/FVC = ratio = percent exhaled within first second
FEF25-75 = forced expiratory flow: the % exhaled between 25%-75%
PEFR = peak expiratory flow rate: highest at first because of mechanical advantage and traction of airways; also a measure of effort
Lung Volumes
- VC = vital capacity
- IRV = inspiratory reserve volume
- TV = total volume
- ERV = expiratory reserve volume
Obstructive and Restrictive Disease Patterns
Lung disease, both obstructive and restrictive, cause FEV1 to be below 80% of expected.
Aide Memoire
oBstructive = Below
- Obstructive diseases cause a FEV1 / FVC ratio below 70%
- Restrictive diseases cause a FEV1 / FVC ratio above 70%
Obstructive disease is characterized by reduced expiratory airflow and not a loss of lung capacity. Accordingly, they have a higher FVC than restrictive diseases. Examples of obstructive diseases include:
Obstructive disease severity is determined by FEV1. |
Restrictive diseases also reduce FEV1 and FVC but have a normal or increased ratio, as FVC can be markedly reduced through a restriction in avalaible lung volumes. These patterns are caused by diseases in the:
Restrictive disease severity is determined by TLC. |
If the ratio is below 70% and the FVC is low, ie below 80% predicted, it suggests a combination of obstructive and restrictive disease, or obstructive disease with hyperinflation.
In early obstructive impairments, FEF 25%-75% may be the first value to become abnormal, and obstructive diseases also have a smaller expired volume (hyperinflation).
Large airway obstruction appears as a flattened inspiratory (intrathoracic) or expiratory (extrathoracic) loop.
Flow Volume Loops
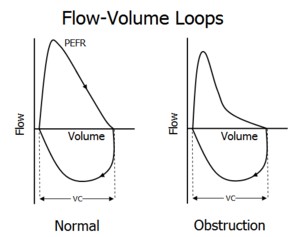 Expiratory flow limitation causes the linear portion of expiratory flow in the normal loop.
Expiratory flow limitation causes the linear portion of expiratory flow in the normal loop.
Scalloping occurs with obstructive diseases, such as asthma or COPD, due to increased lung compliance.
Values are compared with normal values on the basis of age, sex, height, and race.
