
Urine Culture
last authored: Feb 2010, David LaPierre
last reviewed:
Introduction
Urine culture is performed to diagnose urinary tract infection and identify causative organisms. It can also be done to monitor colonization after catheterization.
|
|
Known pathogens
Grow well on routine media:
|
Do not grow well on routine media:
|
|
Procedure
- collection
- dipstick analysis
- culture
- interpretation
Collection
A clean-voided midstream collection is ideal. This involves cleaning of the external genitalia and maintaining asepsis. A midstream is necessary to reduce the contamination by urogenital flora.
Other options include:
- catheterization
- cystoscopy
- nephrostomy
- suprapubic aspiration
Proper storage and transport are critical. Attempt to have urine reach the lab within 30 minutes. If this is not possible, store at 4 C or on ice.
The requisition should contain complete information about the patient, including:
- collection time and method
- clinical presentation
- dipstick results
- current antibacterial therapy given, if any
This will ensure the lab performs the right level of testing.
Dipstick Analysis
Dipsticks can be helpful for point-of-care identification of the presence of infection. The most relevant tests include:
- leukocyte esterase
- nitrates
Culture
Specimens should be processed as soon as possible, or refrigerated for up to 24h. If specimens are received more than 2 hours after collection, without evidence of refrigeration, they should not be processed. However, neither should they be discarded without consulting the ordering physician, as the sample could hold critical value.
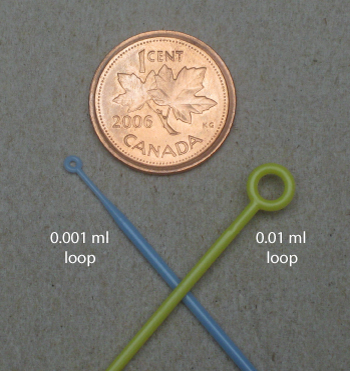
Cultures may be plated by 0.001 ml loop or 0.01 ml loop.
Cultures are plated onto BA and often MacConkey plates, but chocolate or CNA plates are also often used.
Some labs plate all samples onto BA and MacConkey plates, while others will use MacConkey only if the urine is cloudy. This saves on wasted plates.
Routine Cultures
Plated onto 5% sheep blood agar (BA) and a MacConkey plate. Incubate >16h at 35-37 C.
Surveillance Cultures
CNA plate should be added for enterococci, other gram positives, and yeast. Incubate for 48h at 35 C.
Special Cultures
chocolate, CNA plates: 5% CO2 for 48h.
Interpretation
Workup depends on lab and on agreement between lab and clinical staff. Too much workup can lead to wasted resources and unnecessary antibiotics, while too little workup can lead to missed diagnoses.
Isolation of more than two organisms suggests contamination and requires a repeat.
In special cases, such as repeated infections, molecular techniques such as PCR can be helpful at identifying specific microbial genotype.
If pathogenic bacteria are suspected, continue. If non-pathogenic bacteria, can report as normal flora.
Normal flora, or contamination, is diagnosed if:
- <10,000 CFU/L of a given organism
- many organisms
>100,000 CFU/L most likely indicates infection
10,000-100,000 CFU/ml requires clinical evaluation, if there is one organism that predominates
The video will go through identification and sensitivity of the following:
E. coli
|
Enterococcus
|
yeast
|
Evening plates bacteria should be grown for 16-18h. As a result cultures arriving in the evening will need to be read during the afternoon of the next day for optimal reporting.
