
Bipolar Disorder
last authored: Sept 2009, David LaPierre
Introduction
Bipolar disorder is a psychiatric condition in which patients experience disruptions in mood extremes.
Bipolar I disorder is defined as at least one manic or mixed episode (see definitions below); at least one major depressive episode is common but not required.
Bipolar II disorder is defined as at least one hypomanic and at least one major depressive episode; people spend over 50% of their lives depressed.
BD is now occurring more often and earlier globally, possibility due to the destabilizing world we live in, or possibly due to the evolving human mind. The lifetime risk of 0.5-1.5%, and the most common age of onset is 15-25 years. Over 90% of those with manic episodes have future episodes. Common comorbidities include anxiety disorders, substance use disorders, ADHD, eating disorders. Bipolar disorder can be a devestating condition, and 10-15% commit suicide, increased during mixed or depressed episode.
The Case of Fred
Fred was a 26 year-old man who is brought to the emergency department by his wife, who is very concerned by his behaviour.
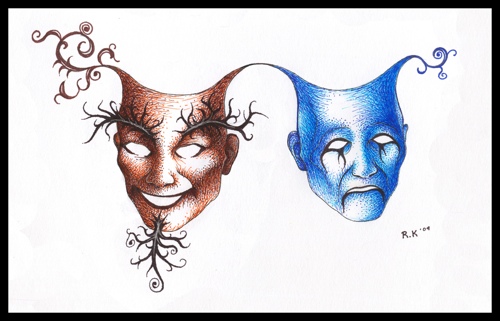
Fraternal Twins by Robert King
Over the past 10 days he has largely stopped sleeping, staing awake studying books on 'beating the system'. He spends at least 5 hours daily at the casino and has lost thousands of dollars.
Questions:
What could be happening?
What do you ask him?
What do you do?
Causes and Risk Factors
In children at highest risk (those with bipolar parents), initial manifestations appear to begin even before puberty. These include anxiety, sleep disturbance, leanring disorders, ADHD, and cluster A traits.
**It would be good to have a diagram here outlining progression from childhood to mania.**
**Three subtypes of BD include typical BD (manic depression), psychosis spectrum, and character disorder**
Triggers
At first, stressors usually precede episodes, acting as triggers. It is thought that kindling occurs over time, with no triggers required as the illness progresses. Triggers include:
- stimulants/street drugs/alcohol
- irregular sleep patterns
- antidepressants: starting or switching
- pregnancy
- life stressors
- abrupt discontinuation of effective mood stabilizers
- nothing
Genetic Influence
Family history is the strongest risk factor (7-12% risk; RR = 8-12), and twin/adoption studies suggests genes are strongly involved, moreso than environment (60-70% for MZ twins). Manifestations in children are affected by the nature of the condition in adults, including variables such as:
- response to lithium
- propensity for psychotic symptoms
- age of onset
- clinical course
No specific genes identified conclusively; likely oligogenic trait, with additive effects.
Signs, Symptoms and Diagnosis
Primary care providers, especially family physicians and emergency room physicians, are often the first point of contact for patients with mania or hypomania. Once suspicion is raised and referral to psychiatry is made, adequate time should be given to sufficiently understanding the details of signs and symptoms, past and present.
- episodes
- history
- psychological testing
- lab testing
A manic episode is a period of abnormally elevated, expansive, or irritable mood lasting at least one week or requiring hospitalization. It is severe enough to cause marked impairment in occupational functioning or in relationships with others, or includes psychotic features.
A hypomanic episode is a period of abnormally elevated, expansive, or irritable mood lasting at least four days. Change in function is not severe enough to cause marked impairment in social or occupational functioning, or to necessitate hospitalization.
Both manic and hypomanic episodes require the presence, to a significant degree, of at least three of the following symptoms:
memory aide: DIGFAST
- Distractibility
- Indiscretion: pleasurable activities with painful consequences
- Grandiosity or inflated self-esteem
- Flight of ideas
- Activity increased, with goal-directed impulsivity or psychomotor agitation
- Sleep
- Talkativeness
Rapid Cycling occurs when four or more episodes per year are present. It occurs in up to 15-20% patients, and is associated with females, antidepressants, middle age, mental retardation, hypothyroidism. Treat with thyroid medication, regardless of lab tests.
History
Fully ouotline ourse of illness
- episodic, without residual symptoms
- onset of symptoms before age 12
Family history
- draw out tree and ask about specific criteria: BD and other conditions, substance abuse, suicide, medications, hospitalizations
Initial questions include:
- patient's expectations
- patient's symptoms and predicament
- collective plan of assessment
- detailed history
- dailiy ratings of mood, anxiety, enery, sleep
- comorbidity
- collateral, including family and past medical records
- labs
Psychological Testing
MMPI?
Lab Testing
Rule out medical conditions through the following tests:
- hyperthyroidism
- anemia
- estrogen, progesterone, and prolactin in women
- vitamins: B12, vitamin D, folic acid
Blood levels of any current mood stabilizing medications.
Differential Diagnosis
Between 40-70% of patients with bipolar disorders are misdiagnosed (ref).
Other causes to rule out include:
- intoxication
- delerium
- hyperthyroidism
- vitamin deficiency (which ones?)
- ** others
Treatments
Immediate Stabilization
Assess safety/functioning and establish treatment settings.
Discontinue antidepressants, caffeine, alcohol,and illicit substances.
Rule out medical causes, including delerium, etc.
Medical management
First-line mood stabilizers include lithium, valproic acid, lamotrigine, olanzepine, or quetiapine.
Some clinicians beleieve multiple drugs should be added together until therapeutic benefit is reached; others believe rational selection and optimization are the best way to proceed. The fact that some patients respond excellently to one drug but not others suggests patient profiles can be helpful in determining initial medication.
Lithium
|
Atypical antipsychotics
|
Lamotrigine
|
If this treatment fails, check adherence, optimize, then try another first line agent.
Treatment of depression (ie with antidepressants) must be done very cautiously to avoid switching to mania.
ECT can also be used.
Lithium is safest during pregnancy, though carries a slight risk of Epstein's cardiac malformation.
Psychosocial support
It is important to discuss triggers with people who have suffered manic or hypomanic episodes. Responsible use of alcohol and drugs, including caffeine needs to be discussed, as does sleep hygience
Psychotherapy can include cognitive behavioural therapy. Behavioural strategies/rhythms and psychoeducation are very useful.
Quitting drugs and alcohol, which can be powerful triggers, is important to consider.
Occupational training/leave from school/work; , substitute decision maker for finances,
Sleep hygeine, social skills training.
Course and Prognosis
It can be very difficult to predict course of illness, and the untreated course is extremely variable.
The duration of an episode is usually 1-6 months, and the median number of episodes is 9.
Good prognosis: short episodes, good quality of remission, advanced age of onset, good premorbid functioning
Over time, cycles may shorten
variability of intervals between epidodes is small in people but can be large among individuals. Some people have their own rhythm and follow distinct patterns
Patients with BD have increased mortality primarily due to suicide. Other increased risks of death include accidents and respiratory disease.
Additional Resources
