
Clostridium difficile
last authored: April 2012, David LaPierre
last reviewed:
Introduction
Clostridium difficile, or C. difficile, is an important bacterial pathogen, representing one of the most significant hospital-acquired infections.

Pseudomembranous colitis (via endoscopy), used with permission
Infection normally follows antibiotic exposure and then contamination, leading to diarrhea, cramps and other symptoms.
Most cases are mild and self-limiting, but more severe infections can lead to an inflammatory condition called pseudomembranous colitis, shown at left.
Even more serious is a complication termed toxic megacolon, which can lead to perforation, peritonitis, sepsis, and death.
The Case of Jacob M.
Jacob is a 42 year-old man who presents to the emergency department with diarrhea and abdominal cramping. His symptoms have been present for one week and worsening.
- Q: what questions do you ask him?
Epidemiology
Five to ten percent of the population is colonized, though this may In one study, hospital carrier rate is 20-50% (ref).
Classification and Characteristics
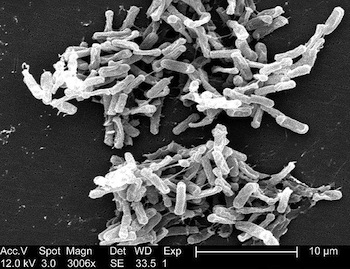
C difficile electron micrograph, courtesy of CDC PHIL #6260
C. difficile is a gram-positive, spore-forming anaerobic bacillus. It was first described in 1935. It received it's name due to it's difficulty being cultured.
C. difficile produces A and B toxins, also known as enterotoxin and cytotoxin, respectively. Both are responsible for degradation of the gut mucosa, attraction of inflammatory cells, and diarrhea.
The BI/NAP1 strain is a more virulent form.
Transmission and Infection
Spread is normally by the fecal-oral pathway, with hospitals being one of the most common sources for transmission. Unfortunately, spores can survive for months in the environment, such as on surfaces.
Exposure to antibiotics is the most important risk factor. While almost any antibiotic can cause C difficile (with the exception of aminoglycosides) the most important offending agents include:
- clindamycin
- fluoroquinolones
- broad spectrum cephalosporins
- penicillin
- macrolides (occasionally)
- trimethoprim-sulfamethoxazole (occasionally)
Other risk factors include:
- hospitalization and long length of stay
- advanced age
- severe illness
- gastric acid suppression (controversial)
- nasogastric intubation
- GI surgery
- cancer chemotherapy
- idiopathic
It appears that disruption of the normal gut flora is the first step in the majority of infections. The disease process therefore normally starts with antibiotic exposure, with infection then following. The bacteria release toxin A (enterotoxin) or toxin B (cytotoxin). Toxin A damages cellular cytoskeleton and leads to leukocytosis.
This leads to mucosal injury and inflammation. Apoptosis.
Prevention
Prevention follows two different strategies:
Reducing infection
|
Reducing colonization
|
Clinical Manifesations
Clincial syndromes are diverse. Many people act as carriers, with no symptoms.

Toxic megacolon, used with permission
Symptoms can include:
- diarrhea, usually watery and foul, up to 10-15x/day; may be bloody
- nausea and vomiting
- abdominal cramping
- fever
- tenesmus (sensation of incomplete emptying)
- myalgia
Pseudomembranous colitis results when C difficile infection leads to more severe disease, with pseudomembranes representing inflammatory debris with a greyish colour that hide the bowel wall.
Fulminant colitis may follow, with severe pain, fever, ileus, and toxic megacolon. This can be a life-threatening condition, leading to perforation, peritonotis, and septic shock.
Diagnosis
When approaching a patient with significant diarrhea, especially one who appears quite unwell, consider bloodwork such as CBC, lytes, BUN, creatinine, as well as 3 views of the abdomen. On the latter, thumbprinting and colonic distension may be seen.
Diagnosis may be made using immunoassay or cytotoxin testing. Immunoassay, which uses ELISA to look for toxins, is the most rapid technique.
Tissue culture testing for cytotoxicity takes longer and is more labour intensive. In this technique, stool is filtered, centrifuged, and treated with broad-spectrum antibiotics to kill all bacteria. The resulting supernatant is incubated with two wells of tissue culture cells, one treated with antitoxin against the cytotoxin (1) and one with only supernatant (2). Cell death in B, but not A, suggests the presence of toxin.
Culture and PCR are rarely used outside of the research setting.
Endoscopy is indicated if diagnosis needs to be made urgently.
Treatment
Treatment should only be offered if disease manifestations are present, regardless of testing results.
Treatment principles include:
- stop the offending antibiotics, and choose a different agent if possible
- implement contact precautions
- provide supportive measures, including fluids and electrolyte replacement
- avoid loperamide and opioids
- curative antibiotics include metronidazole (PO or IV) or vancomycin (PO) for 10-14 days.
Relapse rates are high, especially after many infections. Relapses may be treated with longer treatment regimens. Rifaximin may be used as well.
There is some evidence that probiotics (eg Saccharomyces boulardii) may be useful in preventing disease-associated symptoms, though ongoing treatment is likely required.
For severe, acute cases, vancomycin and metronizazole together should be given. Vancomycin enema may also be used. Surgical consult for subtotal colectomy.
For chronic, refractory cases, fecal bacteriotherapy is one potental treatment option. Stool from relatives are taken, purified, and given by nasogastric tube to the patient to help re-establish normal microflora.
Resources and References
Aslam S et al. 2005. Treatment of Clostridium difficile-associated disease: old therapies and new strategies. Lancet Infectious Diseases. 5:549-57.
Bartlett JG. 2006. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med. 145:758-64.
