
Streptococcus pyogenes
last authored: Feb 2010, David LaPierre
last reviewed:
Introduction
throat swab, courtesy of CDC PHIL
S. pyogenes, or group A Strep (GAS), is a gram-positive bacteria causing a wide range of serious disease, including pharyngitis, cellulitis, meningitis, brain abscess, endocarditis, and necrotizing fasciitis.
It is also responsible for more serious diseases such as necrotozing fasciitis, Toxic shock syndrome, scarlet fever, and rheumatic fever. It can also cause various soft tissue infections.
GAS usually causes intense local inflammation and damage, while toxins it produces can also cause systemic effects.
The wide array of virulence factors allow S. pyogenes to degrade tissue proteins and spread. Particularly effective enzymes lead to organisms responsible for necrotizing fasciitis and myositis.
The Case of John R
John is a five year old boy who develops a sore throat and fever. He visits the doctor two days later and is prescribed a ten course of antiobiotics, but starts feeling better after three days and stops taking the drugs.
One week later, he develops a rash and pain in his knees and ankles.
what is happening to John?
Epidemiology
Strep pyogenes is found throughout the world. Disease is most common in preschool-age children, causing pharyngitis and skin infections (pyoderma). Pyoderma is most prevalent in tropical climates or when the weather is warm and moist.
Asymptomatic colonization of the pharynx and skin is very common, occurring in up to 20% of school-age children.
Good personal hygeine decreases skin colonization, but prevention is difficult due to its prevalence.
Classification and Characteristics
Strep pyogenes is a gram positive coccus which grows primarily in chains.
It is predominantly beta hemolytic, meaning it leads to areas of clear lysis on blood agar plates.
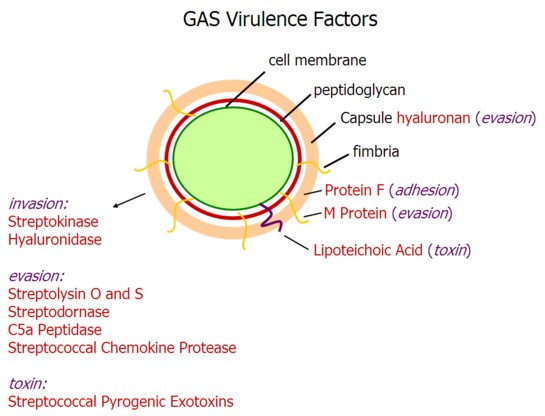
Virulence Factors
hyaluronic acid capsule: evades immune response via molecular mimicry
protein F: mediates adhesion to fibronectin
M protein: prevents phagocytosis
streptokinase: cleaves plasminogen to activate plasmin, dissolving clots |
streptolysin A and O
streptodornase: degrades extracellular DNA used in neutrophil traps C5a peptidase
streptococcal chemokine protease: degrades neutrophil chemotaxin
lipoteichoic acid: released during lysis; triggers cytokine storm and potentially endotoxic shock
streptococcal pyrogenic exotoxins (SPE) A,B,C : act as superantigens by binding non-specifically to immunoglobulin, responsible for toxic shock-like syndrome |
Transmission and Infection
Spread often occurs from asymptomatic carriers, and can be via respiratory droplets and skin-to-skin.
Transmission via fomites and insect vectors are also possible
For soft tissue infections, a break in the skin is required. This can occur with:
- wounds, even minor
- varicella lesions
- bites
- eczema
Pharyngeal infections occur through bacterial adhesins (lipoteichoic acid, protein F) binding to pharygeal fibronectin. Infection usually remains local, but can rarely cause a peritinsillar abscess (quincy). The middle ear or mastoid can also be infected.
Clinical Manifesations
4 S and 4 P
pharyngitis (strep throat)
erysipelas
cellulitis
impetigo (pyoderma): epidermal infection
necrotizing fasciitis
myositis
|
scarlet fever
toxic shock
glomerular nephritis
Rheumatic fever is a multisystem inflammatory disease occuring in the weeks after GAS infection. |
Diagnosis
Diagnosis of skin infections can often be made on clinical grounds.
Pharyngitis can be more difficult to diagnose, though clinical criteria can be helpful.
A throat swab is usually done if suspicion exists, leading to:
- rapid strep tests (specific, but not sensitive; works via detection of group A carbohydrate antigen)
- culture on blood agar plates (may take up to three days)
Serologic testing: anti-streptolysin O titre (ASOT)
- anti-DNase more useful in epidermal infections.
Patients with glomerular nephritis have decreased urine output but increased protein excretion; RBC casts form as they clump together
Treatment
The main reason to quickly treat GAS infection, with a full course, is to prevent the development of rheumatic fever. This should occur before a full immune response.
S. pyogenes is very sensitive to penicillin, and resistance is almost unknown. A ten-day course is recommended.
A single-dose of long-acting benzathine penicillin is also feasible. Erythromycin, other macrolides, or an oral cephalosporin are used in patients with penicillin allergy.
Add clindamycin to toxin-mediated disease in order to prevent protein production.
Rheumatic fever can worsen with future infections by GAS; as a result, people are often given prophylactic antibiotics (penicillin) for many years in patients with this condition.
AHA 2007 guidelines have altered when prophylaxis is given, recommending prophylaxis (oral amoxicillin first choice) for dental procedures if:
- prosthetic valves
- previous endocarditis
- 3 types of congenital heart disease
- cardiac transplant
