
Chronic Abdominal Pain
last authored August 2009, Dave LaPierre
Introduction
"Chronic abdominal pain is a clinical situation requiring as much tact, diplomacy, and compassion as it does scientific knowledge." (Bliss and Wolfe, Cecil's 2007)
The most common diagnosis is "nonspecific abdominal pain", usually a self-limited condition with no identifiable cause.
Differential Diagnosis
Chronic abdominal pain is a common problem, accounting for about 40% of visits to gastroenterologists. Chronic pain can be intermittent, with pain-free periods.
- functional bowel disorders: irritable bowel syndrome
- celiac disease
- chronic depression
- esophagitis
- gastric cancer
- peptic ulcer disease
- disorders of gastric emptying
- subacute outlet obstruction
- constipation
- inflammatory bowel disease
- hepatic tumour, abscess
- hepatitis
- pyelonephritis
- chronic pancreatitis
- pancreatic carcinoma
- chronic cholecystitis
- chronic appendicitis
- intestinal malignancy
- tuberculosis
- mesneteric ischemia (abdominal angina)
- gynecological causes: endometriosis, pelvic inflammatory disease
- ovarian cyst
- Meckel's diverticulum
- AAA
- lymphoma
- diverticulitis
- adhesions
History and Physical Exam
Ninety percent of diagnosis comes from history.
- history
- physical exam
History
red flags
age <5
fever
localization away
from midline
anemia
rectal bleeding
rash
pain at night
travel history
prominent vomiting
and diarrhea
weight loss or FTT
joint pain
ChloridePP
Character: colicky pain builds and subsides, suggesting hollow organ pain. Sharp, stabbing pain suggests peritoneal involvement.
Colicky pain - coming and going - tends to be visceral, ie gallbladder, ileum, ureter.
A constant, localized pain points towards somatic peritoneal origin, with causes including inflammation or infection - pancreatitis, cholecystitis, or appendicitis.
Location
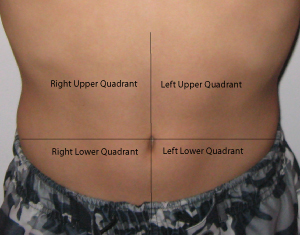
epigastric pain can come from the stomach, duodenum, or pancreas.
right upper quadrant pain can come from the biliary tree or liver (cholecystitis)
periumbilical pain can come from the small intestine, appendix, or colon.
sacral pain can come from the rectum.
hypogastric pain can come from the colon, bladder, or uterus.
Onset: sudden onset can accompany
Radiation: Pancreatic pain tends to radiate through to the middle of the back. Gallbladder pain tends to radiate around to the right side. Renal pain starts in the flank but can radiate to the groin.
- back pain - retroperitoneal causes: aortic aneurysm, pancreatitis, posterior duodenal ulcer, or pyelonephritis
- sacral or pelvic pain: ovarian cysts, PID, pelvic abscess, ectopic pregnancy
Intensity: rate from 1-10, with 10 being the most severe pain the patient has experienced.
- Severe pain suggests ischemia or infarction, or generalized peritonitis (ie perforation)
Duration: waves of pain suggest rhythmic muscle contractions, such as those of peristalsis, are involved.
Events Associated: A pertinent review of systems based on the differential.
Provoking and Palliating Factors: The impact of certain behaviours can point to system of origin. Changes with eating, bowel movements, or vomiting suggest pain is GI in origin. Increased pain with exertion suggests cardiac causes.
Associated Symptoms
- fever and chills: inflammation or sepsis
- distension or bloating: intermittent with IBS, progressive with mass or ascites
- weight loss: malignancy or IBD
- change in bowel habits: malignancy
- rectal bleeding
- nausea/vomiting: pain reflex, gastroenteritis, bowel obstruction
- jaundice: liver, biliary tree, gallbladder or hemolysis
- vaginal discharge: PID
past history
- previous episodes
- previous surgery
- medications
- constipation (potentially leading to obstruction)
Physical Exam
The physical exam can reveal important clues, and should be started with simple inspection of the state of the patient. Weight loss, pignmentation, and signs of dehydration are all possible.
Auscultation can be used to assess bowel sounds and discover bruits.
Palpation should be done gently, starting away from area of pain. Percussion can be used to measure organ size and determine presence of ascites. A pulsatile mass suggests aneurysm, and peripheral pulses should be felt.
Peritonitis is an important finding, first suspected with pain, involuntary guarding or rigidity while taking a deep breath (the most sensitive test). Percussion tenderness may be provocative. Absent bowel sounds are usual, as is rebound tenderness (though this is an inhumane test; avoid it).
Right upper quadrant pain can sometimes be associated with a palpable mass in Crohn's disease.
Rectal examination is important to rule out tumour obstruction.
Pelvic examination should be done to rule out pelvic infammatory disease.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
CBC: signs of infection, anemia, lymphoma
liver labs: hepatic or biliary tract involvement
coagulation profile: especially important for people on anticoagulants
electrolytes, glucose: ketoacidosis, hypercalcemia
amylase and lipase: pancreatitis
b-HCG for pregancy
arterial blood gases: metabolic acidosis in ischemia, peritonitis, pancreatitis
urinalysis and renal function
fecal occult blood test: upper GI bleeds
Diagnostic Imaging
ECG: MI
CXR: free gas, pneumonia
abdominal X-ray: chronic pancreatitis, constipation
ultrasound: intra-abdominal abscess, gallstones, chronic cholelithiasis, ovarian cyst, AAA, renal tumour
endoscopy: peptic ulcer disease, gastritis, or tumours
colonoscopy: diverticulitis, colonic ischemia
CT: pancreatitis, pancreatic carcinoma, AAA, diverticulitis
IVU: stones, renal tumours
ERCP: chronic pancreatitis, pancreatic carcinoma
small bowel enema: Crohn's disease, Meckel's diverticulum
HIDA scans can be used to evaluate gallbladder conditions, but takes time
Pathophysiology
Abdominal pain results from thermal, mechanical, or chemical stimulation of specific sympathetic nervous system receptors. Visceral neurons are C type, resulting in variable sensation and localization. Peritoneal pain is carred by A and C types, resulting in sharp, localized pain.
Abdominal pain can step from structures in the gastrointestinal, cardiovascular, peritoneal, musculoskeletal, and pelvic systems.
Parietal PainParietal pain originates in the parietal peritoneum and is caused by inflammation. Steady aching pain is more severe than that of visceral pain and can be more precisely localized, as it is carried by somatic nerves. It is typically made worse by movement or coughing, and people tend to want to lie still. Rebound tenderness is present.
|
Visceral PainVisceral pain originating in internal organs and structures tends to activate vagus and splanchnic autonomic nerves, with diffuse difficult to localize, typically midline pain. If mucosal, pain tends to be steady - if crampy, visceral pain suggests intraluminal problems.
|
Referred PainReferred pain originates at one location but is felt in another site, superfically or deeply, within or near the same spinal level(s). Abdominal pain can be referred from the thorax, abdomen, pelvis, or spine.
|
Clinical Vignette 1
A person takes this treatment for this reason due to concerns re: condition
This happens.
How do you respond?
Clinical Vignette 2
Additional Resources
Topic Development
created: DLP, Aug 09
authors: DLP, Aug 09
editors:
reviewers:
