Wound Care
last authored: Dec 2009, David LaPierre
last reviewed:
Introduction
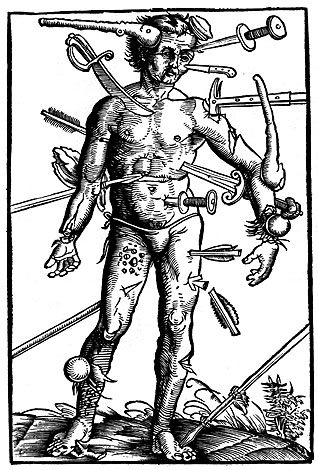
Wounds are extremely common as a product of daily living. They range from the inconvenient to the life-threatening, as can occur during trauma, as depicted in the image below.
Wounds can also be created during health care, such as following biopsy or in surgery.
Wound care is an important component of first aid and should be understood by members of the public. Many wounds, such as minor cuts and scrapes, can effectively be dealt with at home. This primarily includes cleaning, basic hemostasis, and dressing, as well as monitoring for signs of infection.
Other wounds require attention of various health care providers, who should understand important principles to save life and limb, prevent infection, offer comfort, and maintain function and appearance.
Chronic wounds can require substantial time and efforts for their healing, which is not always successful. These can arise as complications of diabetes, venous stasis ulcers, and other conditions.
Many health care providers are involved with wound care, including physicians, nurses, and home care workers.
Clinical Evaluation
It is important to assess a number of factors regarding the cause and background of the wound to determine ideal treatment.
- history
- physical exam
- imaging
History
Mechanism of injury can determine degree of injury and risk of infection.
When did the wound occur? Bacterial proliferation can lead to serious complications. A wound may be sutured up to 8 hours after injury, or up to 24 hours if on the face or scalp.
Past medical history: any conditions predisposing to more serious conditions (diabetes, splenectomy, etc)
Last tetanus shot
Allergies to anesthetics
Physical Exam
Any other more serious injuries?
Describe wound as completely as possible, including shape, length and depth.
Observe for foreign materials or clearly dead tissue.
Assess integrity of bones, nerves, tendons, and blood vessels prior to wound exploration.
Imaging
If warranted and available, imaging can be useful for identifying foreign bodies and tissue damage. X rays can point to bony injury or foreign material such as metal, while ultrasound can reveal organic matter such as wood.
Decontamination
In order to reduce the risk of infection, it is imperative that all wounds be as free as possible of bacteria, regardless of the chosen method of wound closure. The best method for the prevention of wound infections remains prompt and thorough wound care, debridement and cleansing.
Cleanse the Surrounding Skin - a variety of antimicrobial agents may be used to cleanse the area around the wound. One of the most effective and commonly available is Povidone - Iodine 10% Solution. Others include Chlorhexidine, Alcohol and Soap Solutions. While these agents are safe and effective on intact skin, they must not be used on the open wound. Their short-term antimicrobial effect is offset by direct tissue damage and impairment of local leukocyte activity - the result in most cases being an increased risk of infection.
Remove Gross Debris - the next step in wound decontamination (after anaesthesia) is to remove any large pieces of dirt or debris. This is accomplished with a pair of forceps (expensive tweezers). Sometimes it is impossible to remove every fragment of foreign material. In general, it is safer to leave small fragments of inert material, such as metal or glass, than to neglect organic matter such as wood or bone. The physician must weigh the risk of infection against the risk of aggressive wound exploration and tissue damage.
Mechanical Scrubbing - although advocated by some, scrubbing an open wound may cause tissue damage and therefore increase infection risk. Recently, very fine porosity sponges have been developed which cause less damage to exposed tissues. Unfortunately, these are not always easily available. Mechanical scrubbing is best reserved for contaminated wounds in which high pressure irrigation (see below) is unsuccessful in removing all debris. More information is available at debridement.
Wound Irrigation - the preferred method of removing small particulates and bacteria from an open wound. In the operating room this may be accomplished using sterile normal saline and simply pouring the solution over the wound, or in some circumstances the wound may be flushed using a bulb syringe. Rarely would the wound be irrigated with sterile water. In the outpatient setting, however, irrigation may be achieved using copious amounts of sterile water or sterile normal saline and pouring it over the wound. Depending on the wound size and degree of contamination, the volume of solution used may range from 200 cc to several liters. Irrigating wounds using solution under pressure may cause further damage to the tissue.
Antibiotics - Although antibiotics are often given prophylactically to patients with 'high risk' wounds, the scientific evidence supporting this practice is weak in most circumstances. Antibiotics are commonly used for animal bites, dirty or grossly contaminated wounds, late presentations etc. There are too many variables to consider here - the reader is referred to more detailed texts for a full discussion of the risks and benefits.
Wound Closure
Most wounds should simply be allowed to heal on their own, with no care other than keeping it clean and dressed. In more serious wounds, including those inflicted as a part of health care, closure is required. Wound closure has a number of benefits and risks:
benefits
|
risks
|
Primary closure is the cleaning and closure of a wound at time of presentation. Suturing is a common means of closing wounds.
Secondary intention is the cleaning/debriding/packing of a wound at time of presentation, but not its suturing. The wound is frequently assessed for infection and to change packing. It is preferred for wounds that are infected, or are at high risk of becoming so. The wound heals through natural wound healing.
Delayed primary closure is the cleaning/debriding/packing of a wound at time of presentation, but the deferral of suturing for 3-5 days. It is performed in cases of high infection risk but when cosmetic or functional results are important.
Ongoing Care
The ongoing care required depends heavily on the nature of the wound. The simplest requires noting other that clean conditions and monitoring by the patient. Sutures are at times resorbable, but can require follow-up for their removal. More complex wounds, particularly those healed by secondary intention, involve ongoing dressing changes to control infection and facilitate closure.
Additional Resources
Association for the Advancement of Wound Care - Guidelines