
Lipid Transport
last authored:
last reviewed:
Introduction
Lipids are transported in the blood bound to various lipoproteins, which are spherical complexes of lipids and apoproteins. Lipoproteins transport lipids throughout the body and keep them soluble as they do so.
Lipoproteins are composed of a lipid core, containing TAG and cholesterol esters, and an outer shell made up of amphipathic apoproteins, phospholipid, and nonesterified cholesterol. Lipoprotein contents are constantly being passed from one to another, making the distinction between classes somewhat variable.
They include chylomicrons, very-low-density lipoproteins, low-density lipoproteins, and high-density lipoproteins. These differ in size, composition, and density.
As we age, lipoproteins gradually build up in tissues and contribute to atherosclerosis.
Composition |
Apo proteins |
Lipids |
||
|---|---|---|---|---|
Chylomicrons |
mostly TAG |
B48, C-II, E |
|
|
VLDL |
50% TAG |
B-100, C-II, E |
|
|
LDL |
50% cholesterol |
B-100 |
||
HDL |
50% protein |
A, C, E |
Chylomicrons
Chylomicrons are assembled in intestinal mucosal cells and contain TAG, cholesterol, and fat-soluble vitamins.
Apoprotein B-48 is unique to chylomicrons. It is termed B-48 because it contains only 48% of the entire apo B protein. During apo B-48 movement from the ER to the Golgi, it is loaded with lipid. This forms secretory vesicles that fuse with the plasma membrane and are released into the lymphatic system.
Once in the plasma, chylomicrons receive apo E (for liver recognition) and apo C-II (for activation of lipoprotein lipase).
The TAGs in chylomicrons are cleaved by lipoprotein lipase, once activated by apo C-II, predominantly in the capillaries of adipose and muscle tissues. Lipase is attached to the endothelial lumen via heparan sulfate chains. Deficiency of lipoprotien lipase or apo C-II causes Type I Hyperlipoproteinemia, a rare recessive disorder.
Lipoprotein lipase synthesis and lumenal expression is increased by insulin. Heart lipase has a lower Km than adipose lipase, allowing it to access circulating TAGs even when levels are low.
FFAs can directly enter adipose or muscle cells for storage or energy, or can be transported on albumin to other parts of the body. Most cells can oxidize FFAs to produce energy. Adipocytes can re-esterify FFAs to produce TAGs.
Liberated glycerol is returned to the liver, where it is almost exclusively used to produce glycerol-3-phosphate, which can enter glycolysis or gluconeogenesis.
Chylomicron remnants - cholesterol esters, phospholipids, and apolipoproteins - are taken up by the liver via recognition of apo E, where they hydrolyzed and recycled. Apo C-II is returned to HDL.
Very Low Density Lipoproteins (VLDL) & Intermediate Density Lipoproteins (IDL)
VLDLs are produced in the liver and are composed primarily of TAG, which they deliver to peripheral tissues. VLDLs contain apo B-100 when secreted, but must pick up apo C-II and apo E from circulating HDL. Abetalipoproteinemia is caused by a defect in TAG transfer protein, leaving apo B unable to be loaded with lipid. As a reult, no chylomicrons or VLDLs can form.
As VLDLs pass through the circulation, lipoprotein lipase liberates FFAs and the VLDL becomes denser. apo C-II and E are returned to HDL, while apo B-100 is retained. Remaining TAGs are transferred to HDL in exchange for cholesterol esters.
With these changes, VLDLs become IDLs, or VLDL remnants. These can be taken up through endocytosis using apo E as a ligand, or become LDLs.
Low Density Lipoproteins (LDL)
The primary function of LDLs is to deliver cholesterol to tissues. They have much less TAGs, but more cholesterol, than VLDLs. They are normally taken up (endocytosed) by cells across the body. However, when LDL levels are too high (hypercholesterolemia), LDL gets deposited in blood vessel walls.
They do through recognition of apo B-100 or apo E (but not apo B-48) by LDL receptors. These receptors are glycoproteins that are associated with clathrin-coated pits. Following endocytosis, the vesicle fuses with endosomes, the receptors are recycled, and lipid contents are used by the cell. Following endocytosis, LDL receptor expression is downregulated. Excess cholesterol is esterified for storage by acyl CoA:cholesterol acyltransferase (ACAT).
Mutations in the LDL receptor, or in apo B-100, lead to type II hyperlipidemia.
Thyroid hormone, T3, facilitates LDL binding with its receptor. As such, hypothyroidism is a common cause of hyperlipidemia.
A healthy LDL is between 2-4 mmol/L. Target numbers change based on risk factors.
The higher the LDL, the higher the risk of cardiovascular problems (Ballantyne, 1998). Macrophages can endocytose oxidized LDL using scavenger receptors class A (SR-A). Accumulation of cholesterol esters converts macrophages into foam cells, which are important mediators of atherosclerosis
High Density Lipoproteins (HDL)
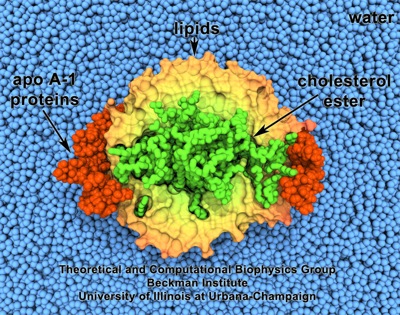
HDL. Made with VMD and owned by the Theoretical and Computational
Biophysics Group, NIH Resource for Macromolecular Modeling &
Bioinformatics, Beckman Institute, University of Illinois, Urbana-Champaign
HDLs are secreted directly into the blood from the liver and intestine, and are important for various functions.
They serve as a reservoir of apo C-II and apo E for transfer to other lipoproteins. Nascent HDLs are disc shaped, but due to their high concentration of phospholipid they rapidly accumulate unesterified cholesterol from other lipoproteins or cell membranes.
This makes them candidate molecules to mop up cholesterol from developing or existing atheromas on vessel walls.
HDL cholesterol is esterified by the enzyme PCAT, and transported to VLDLs. HDLs also transport cholesterol to the liver for disposal or to steroidogenic cells, forming a key component of cholesterol homeostasis. There is thus an inverse relationship between [HDL] and atherosclerosis as it mediates reverse cholesterol transport.
Exercise and moderate alcohol consumption raise HDL levels, while obesity and smoking lower them.
Lipoprotein (a)
Lp(a), is nearly identical to LDL, and when present in large quantities is a risk factor for heart disease. Levels appear to be predominantly mediated by genetics, though lifestyle is also involved. Lp(a) is similar to plasminogen, and it is possible that it contributes to heart attacks by by binding to plasminogen activators and slowing down the breakdown of blood clots.
