
The Case of Smokey Marlborough
last authored: Jan 2010, Sean Doran
last reviewed: Jan 2010, Una Doran
The following case is provided as a means to assist you in generating a "picture of the patient" and an opportunity to think about what you feel are the important questions, pertinent facts, etc. It is also intended to be somewhat fun so please enjoy!
Introduction
You are working in the Emergency Department (ED) of a busy tertiary care center when you are asked to see a patient presenting with a complaint of chest pain. You pick up the RN notes and chuckle when you read the name - Smokey Marlborough. The RN tells you that Mr. Marlborough (hereinafter referred to as Mr. M) is a 62 year old man who was brought to the ED via Emergency Medical Services (EMS) after his daughter called EMS when she became alarmed at her fathers' complaint of chest pain.
Think of what information you would like to obtain immediately (hint: often found on the triage note).
You immediately take a look at the triage vital signs (VS) of Mr. M are. They are as follows: heart rate (HR) 99; respiratory rate (RR) 20; blood pressure (BP) 153/98; and an oxygen saturation of 94% on room air (ORA). Somewhat comforted by these findings, you make your way over to the bedside of Mr. M. When you arrive, you notice that he is looking rather uncomfortable and breathing more rapidly than you expected. Unfortunately, you do not see any cardiac monitors on the patient and thus, have no idea of what his current vital signs or EKG rhythm might be.
What you would like to do next?
You immediately ask the RN to get "cardiac monitors and oxygen saturation" on the patient. While the RN is getting things in order, you take the opportunity to measure the patients pulse and notice that it is now approximately 111 bpm and the respiratory rate has increased to approximately 24 bpm. The RN finished getting cardiac monitors on and you notice and unusual pattern to the rhythm strip as well as lower oxygen saturation of approximately 88%. The automatic blood pressure cup finally displays a blood pressure of 97/62.
At this point in the story, please take a moment to think of two things: (i) a potential differential diagnosis; and (ii) what steps you would like to take next.
You identify the patient as being in shock, likely cardiogenic. Additionally, you quickly run through a brief differential diagnosis of chest pain (in no specific order) - acute MI; spontaneous pneumothorax; aortic dissection; esophageal rupture and pulmonary embolism. Looking at Mr. M you notice that he has a rather ashen looking appearance, is short of breath and is holding a clenched fist over the center of his chest. He is not looking well and you have a strong suspicion that he is suffering from an acute coronary syndrome - specifically, acute myocardial infarction. You complete a rapid assessment of the patients airway, breathing and circulation, order IV access and fluids, and order a stat EKG.
Please note, we have not even discussed any details with the patient. In reality, you would introduce yourself to Mr. M as early as possible in order to gain information regarding his medical history to help refine your differential diagnosis. Also, you would want to assure Mr. M that he is in good hands and that the Emergency medical team is doing everything they can for him.
Nevertheless, I would like to point out how much information was gleaned merely by looking at the patient, considering the limited information provided at triage and his vital signs.
The story contiunes...
As you are waiting for the EKG you order morphine for comfort and oxygen via nasal prongs. Also, you take the opportunity to obtain a history from Mr. M. You first ask when the pain began and he responds "approximately 35 minutes ago". When asked to described the pain, he tells you that it feels like he has a tightness in his chest that is radiating to his shoulder. He reports that he is also feeling short of breath.
What specific information would you like to obtain from Mr. M.?
Cardiac risk factors are crucial to ask any patient presenting with a complaint that could be cardiac in origin. The critical cardiac risk factors are:
(i) age > 45 (male or > 55 female)
(ii) male sex
(iii) prior CAD or MI
(iv) 1st degree relative with MI < 65 (female) or < 55 (male)
(v) lifestyle factors - smoking history, sedentary lifestyle and poor diet
(vi) hypertension
(vii) hypercholesterolemia
(viii) diabetes mellitus.
After obtaining Mr. M.'s history, you realize that he has all of these cardiac risk factors.
The EKG has returned and it looks as follows:
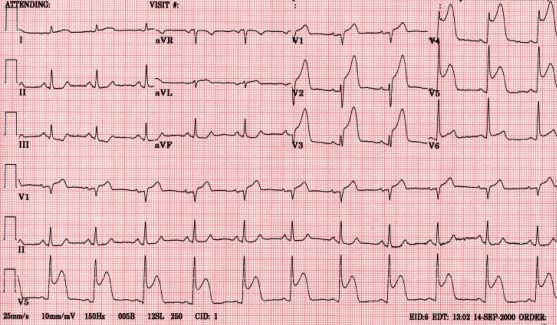
What does the ECG show?
You resist the temptation to immediately jump to the obvious and run through the usual approach - rate, rhythm, axis, deviation, P before every Q, etc. However, once quickly running through your approach you turn your attention to the obvious - ST elevations in leads V1 - V5.
Given the patients clinical condition and EKG you conclude that Mr. M is suffering a STEMI. Remembering the acronym MONA from medical school, you order morphine, oxygen, sublingual nitro spray and an aspirin to chew. You ask the unit clerk to page cardiology immediately and turn your attention back to Mr. M. in order to discuss his clinical situation with him.
