
Sinusitis
last authored: June 2012, David LaPierre
last reviewed:
Introduction
Sinusitis is an inflammation of the mucous membranes of the nasal cavity and paranasal sinuses, with fluid within these cavities and/or the underlying bone.
Rhinoinusitis is an inflammation of the mucous membranes of the nasal cavity and paranasal sinuses, with fluid and mucus collection within these cavities. While disease can predominate in either the nose or sinuses, the terms rhinitis or sinusitis are no longer perferred due to the continuity of these structures.
Acute sinusitis has been present for less than 4 weeks, while chronic sinusitis has been present for greater than 12 weeks. Recurrent disease strikes at least 4 times per year, with each bout lasting at least 10 days.
The Case of Mary S.
Mary is a 34 year old healthy woman. She comes to your office after a three day history of cough, sore throat, and runny nose. She feels this is simply a cold, but is concerned she might have a sinus infection due to the intense pain and pressure she feels below her eyes. These symptoms started this morning. She is asking for antibiotics.
- what further questions do you ask?
- what physical exam do you perform?
- do you give Mary antibiotics?
Causes and Risk Factors
Risk factors include:
- medical conditions such as RTIs, allergic rhinitis, cystic fibrosis, immunodeficiency
- anatomic abnormalities, such as a deviated septum, polyps, adenoid hypertrophy, tumours
- irritants: tobacco smoke, air pollution, chlorine
- drugs: decongestant overuse, cocaine
The most common pathogens include:
viruses: rhinovirus, influenza, parainfluenza
adults:
children:S. pneumoniae, H. influenzae, M catarrhalis
Allergic rhinosinusitis can be perennial, seasonal, or occupational. Common allergens include:
- perennial disease: dust mites, cats, dogs, molds
- seasonal: pollens from grasses, trees, weeds, molds
- occupational: latex
Infective rhinosinusitis may be caused by:
- viruses: rhinovirus, influenza, parainfluenza
- bacteria: S. pneumoniae, H. influenzae, S. aureus, S. pyogenes, Pseudomonas, M catarrhalis, anaerobes, and gram-negative enteric bacteria.
- fungi
Chronic disease can be caused by:
- S. aureus
- anaerobes
- Pseudomonas
- others...
Vasomotor rhinitis is more common in the elderly but can affect anyone.
Non-allergic rhinitis with eosinophelia syndrome (NARES) is seen in ~20% of patients with perennial nasal symptoms and no allergic cause. Asthma is also often seen in these patients.
Medications, including aspirin, oral contraceptives, estrogen, beta-blockers, and ACE inhibitors can lead to nasal symptoms. Rhinitis medicamentosa follows decongestant overuse and rebound edema.
Hormonal rhinitis can be brought out by pregnancy, hypothyroidism, and emotional states, such as anger or sexual arousal.
Other risk factors for rhinosinusitis include:
- medical conditions such as RTIs, allergic rhinitis, cystic fibrosis, immunodeficiency
- anatomic abnormalities, such as a deviated septum, polyps, adenoid hypertrophy, tumours
- irritants: tobacco smoke, air pollution, chlorine
Pathophysiology
Children have only maxillary and ethmoid sinuses by age 6.
Irritants, allergens, or pathogens can be deposited in the ostiomeatal complex and cause mucosal edema. The narrow airways can easily become obstructed, leading to sinus congestion. Mucus retention can lead to increased susceptibility to infection.
Allergic rhinosinusitis is caused by airway inflammation, mediated by eosiniphilia and release of cytokines such as IL-4 and IL-5. Mast cell degranulation leads to histamine release, along with other cytokines.
Viral sinusitis can cause decreased ventilation and increased mucus collection, increasing risk of bacterial sinusitis.
Outflow obstruction may also be caused by mucus stasis, as can occur in cystic fibrosis or immotile cilia syndrome. Other host factors include septal deviation, traumatized anatomy, or surgery.
Bilateral nasal polyposis is often seen along with chronic rhinosinusitis. It has a prevalence of 4%, with increasing incidence with age. Nasal polyps are bags of pale, swollen mucosa, commonly occurring in the ethmoid sinuses and extending through the middle meatus. Polyps can become covered with squamous epithelium over time, appearing fleshy and reddened.
Vasomotor rhinitis is thought to be due to increased parasympathetic activity, leading to nasal secretions and congestion via decreased vascular tone.
Signs and Symptoms
- history
- physical exam
History
A diagnosis of acute bacterial sinusitis can be difficult.
Bacterial sinusitis tends to present with a worsening of symptoms after somewhat of improvement. Other signs suggestive of bacterial infection:
- facial, unilateral pain
- maxillary toothache
- purulent nasal secretions
- poor response to decongestants
- abnormal transillumination
Red Flags
- swollen eye
- displaced globe
- double vision
- ophthalmoplegia
- reduced visual acuity
- frontal swelling
- severe, unilateral, frontal headache
- meningeal signs
- neurological symptoms
Sinusitis
Major criteria:
- nasal blockage/congestion or purulent postnasal drainage
- purulent nasal discharge
- facial pain or pressure
- fever
- reduction in sense of smell
Minor criteria:
- frontal headache
- fever in nonacutre disease
- halitosis
- dental pain
- cough
- ear pain/fullness
Associated symptoms can include:
- sore throat
- sneezing
- itchy eyes
- cough
- malaise
- fever
Inquire into:
- onset, duration, and cycles of symptoms
- triggers (smoke, pets, workplace)
- impact on life
Review of systems should be carried out to evaluate the presence of systemic conditions, such as Wegener's granulomatosis or sarcoidosis.
Physical Exam
Rhinoscopy may reveal polyps. Bilateral polyps are in keeping with this disease; unilateral symptoms should be investigated for malignancy or fungal disease.
Viral rhinitis causes edematous, pale mucosa with copious clear secretions.
Bacterial rhinosinusitis canses swollen, tender mucosa coated with purulent discharge.
abnormal transillumination
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
Allergy testing should be performed for common allergens.
Levels of IgE or eosinophils can also be helpful.
Diagnostic Imaging
All patients with pronounced frontal headaches should have a radiograph to r/o frontal sinusitis
Perform imaging (ie CT) only if the diagnosis is in doubt.
Chronic sinusitis demonstrates CT or MRI.
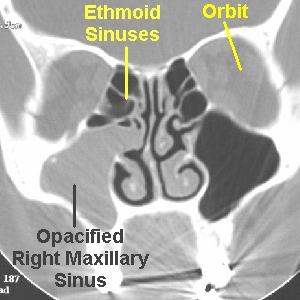
used with permission,
Dr. Ghorayeb, OTOLARYNGOLOGY HOUSTON
While some experts suggest X-ray films are unhelpful due to poor sensitivity and specificity, they do have a role in ruling out sinus disease.
CT of the sinuses can be very helpful in staging disease. MRI is normally only done if malignancy or fungal disease is suspected.
Differential Diagnosis
Rhinosinusitis is often confused with midfacial pain, which can be caused by migraine, tension headache, or trigeminal neuralgia.
A thorough history is crucial to make the distinction.
- subjective experience of obstruction
- polyps
- systemic diseases: sarcoidosis, Wegener's
- deviated septum
- crusting from other infections
- hypertrophied turbinates
- foreign body (consider in unilateral symptoms)
- tumour
CSF leak
- spontaneous
- traumatic
Treatments
Antimicrobial treatment may be beneficial for bacterial sinusitis, but some studies have shown no significant benefit.
First line: amoxicillin , TMP-SMX if allergic to penicillins
Second line: cefuroxime, clarithromycin, ceflacor, cefitime.
If no response is seen after 5-7 days, consider broad-spectrum such as amoxicillin-clavulanic acid, levofloxacin, cephalosporin.
If no response after 3-4 weeks, choose metronidazole or clindamycin for anaerobic coverage.
Other adjuncts that may be helpful include:
- inhaled steam of facial packs
- saline nasal sprays
- oral and nasal decongestants (short time only)
- nasal corticosteriod spray (chronic sinusitis only)
- oral mucolytics (guaifenesin, bromelain
Antihistamines are contraindicated.
Referrals
ENT should be consulted if:
- second-line therapy fails
- > 3 episodes yearly
- development of complications: mucocele, orbital extension, meningitis, intracranial abscess, venus sinus thrombosis
Antimicrobial treatment x10 days can be beneficial, but should only be used after 5-7 days of unresolving symptoms.
- First line: amoxicillin (TMP-SMX if allergic to penicillins)
- Second line: amoxil/clavulin, clarithromycin, ceflacor, cefitime
Chronic sinusitis should be treated with clindamycin or metronidazole.
Nasal corticosteriod spray should be used for chronic rhinosinusitis only.
Adjunct therapies
Saline nasal spray or wash, along with humidification, can be used to clear the upper wairways of allergens and other irritants.
Topical or systemic decongestants can be used, but for a short time only (less than 3 days) to prevent rebound swelling.
Antihistamines are contraindicated for infectious rhinosinusitis, but can be useful for allergic symptoms.
Analgesia can be used for mild or moderate symptoms.
Surgery
ENT should be consulted if:
- second-line therapy fails
- > 3 episodes yearly
- development of complications: mucocele, orbital extension, meningitis, intracranial abscess, venus sinus thrombosis
Surgical management includes FESS, or functional endoscopic sinus surgery. FESS can provide much relief, though recurrences are common as polyps regrow.
Consequences and Course
Up to 40% of patients will recover spontaneously.
Complications, though rare, can include:
- periorbital cellulitis, orbital cellulitis or abscess
- intracranial infection - cavernous sinus thrombosis, meningitis, frontal lobe abscess or osteomyelitis
- aspiration and chronic bronchitis
Resources and References
Allergic Rhinitis and Its Impact on Asthma - see "Documents and Resources" for clinical pocket guide
Topic Development
authors:
reviewers:
