
Dialysis
Dialysis is the removal of waste products and excess fluids following acute or chronic renal failure. There are three types of dialysis - hemodialysis, hemofiltration, and peritoneal dialysis (PD). At best, dialysis provides an average clearance of 10 ml/min, compared with a normal GFR of 120 ml/min.
Indications include:
- GFR <5-10 ml/min
- BUN >30mmol/L
- hyperkalemia refractory to medical management
- acidosis, refractory to medical management
- fluid overload, refractory to medical management
- uremia: pericarditis, encephalopathy, seuzures, bleeding
- poisonings: ASA, methanol, ethylene glycol, lithium, TCAs, theophylline
- hypercalcemia?
- Acidosis
- Electrolytes
- Ingestion
- Overload
- Uremia
During dialysis, urea, phosphate, and other things are taken out, while calcium and bicarbonate added back in.
A semi-permeable membrane filters dialysate solution to regulate fluid and electrolyte balance.
- peritoneal dialysis
- hemodialysis
- hemofiltration
- choosing the right type of dialysis
Peritoneal Dialysis

Peritonaeal dialysis (PD), as the name suggests, uses the peritoneal membrane's semi-permeable characteristics to filter wastes and provide fluid and electrolyte homeostasis.
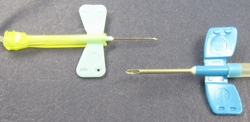
PD uses a permanent catheter, inserted through the abdomenal wall, to transfer fluid to and from the peritoneal cavity. The catheter, shown at left, has multiple holes to increase fluid passage.
Dialysate is tranferred up to 5 times daily, with fresh fluid introduced each time. Solutes move down their concentration gradients, while water is shifted via osmotic drag, provided by dextrose or other solutes.
When starting PD, the quality of a person's membrane is unknown. Perfusion rates are controlled by surface area, vasculature, and amount of peritoneal scarring, and emperic approaches are used to plan future treatments.
Dialysate comes in various concentrations, ie 0.5%, 1.5%, 2.5%, or 4.25%. Concentration used on a given day depends upon fluid status - weight gain/loss, peripheral edema, blood pressure, or symptoms thereof.
PD is used in various settings, including as maitenance for end-stage renal failure. Technique survival decreases to 50% after 5 years due to loss of peritoneal membrane function.
Complications include:
- peritonitis (often due to Staph. epidermidis). Treatment is with intraperitoneal or intravenous antibiotics.
- mechanical blockage of fluid drainage, often by constipation
- infections at catheter site
- pleural effusions or sclerosing peritonitis
Contraindications include:
- peritoneal adhesions following peritonitis
- abdominal hernia
- colostomy
It is important to assess the bag of spent dialysate. Look at clarity, presence of fibrin, and bag weight to learn how much fluid was taken off.
Hemodialysis
During hemodialysis, blood is removed from the body, placed in contact with dialysate fluid through a semi-permeable membrane, and returned to the body, normally for 4h of treatment, 3x weekly. The aim is a 70% reduction in BUN.

Blood leaves either through a fistula or a central line, at ~300 ml/min. Blood flows through a dialysis machine and a semi-permeable membrane, bathed in dialysate fluid, which flows at ~500ml/min. Toxins are removed and important solutes added back in, moving down a concentration gradient.
The goal is to return patients to their dry weight when doing dialysis. When people first present, the may have lost some weight from their condition. Dialysis will improve their status, and as they regain muscle mass, dry weight needs to be shifted upwards.
Arteriovenous fistulas are constructed surgically, usually by joining the radial artery and cephalic veins. The venous system then arterializes, providing access to high blood flows required for dialysis. Fistulas can be susceptible to infection or thrombosis.
Dialysis dose can be adjusted by altering blood flow, changing the area of semi-permeable membrane, or by varying the duration of treatment.
Patients are weighed before dialysis to determine the level of fluid required for removal. Generally, a maximum of 1kg/hour of fluid is removed.
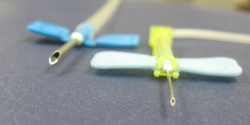
 Blood flows through
the many tubes in the filter, shown on the right. The tubes, composed
of semi-permeable membranes, are bathed in dialysate fluid, and fluid
and solutes pass through the tubes bi-directionally. Blood then flows
out the bottom of the filter before being returned to the body.
Blood flows through
the many tubes in the filter, shown on the right. The tubes, composed
of semi-permeable membranes, are bathed in dialysate fluid, and fluid
and solutes pass through the tubes bi-directionally. Blood then flows
out the bottom of the filter before being returned to the body.
There are various synthetic membranes available, each with different permeability characteristics.
Hemodialysis can result in hyperkalemia and hyperphosphatemia, due to difficulties removing these solutes. Water-soluble vitamins such as Vitamin C and folic acid are also dialyzed out, requiring supplementation.
Complications of hemodialysis include:
- hypotension
- infection
- hemolysis
- air embolysi
- reaction to dialysis membrane
Dialysate fluid

Dialysate fluid is made from purified, non-sterile water with a solute concentraion similar to plasma, but without wastes.
Important solutes added back include potassium
Hemofiltration
Hemofiltration involves filtering the blood across a semipermeable membrane, allowing the removal of small molecules. Fluid is replaced to make up for losses, and is commonly buffered with lactate.
Hemofiltration is commonly used in cases of acute renal failure, especially in the ICU, as slower, continuous filtration causes smaller fluid shifts and therefore hypotension than hemodialysis.
Choosing the Right Type of Dialysis
PD is a gentler dialysis, avoiding the troughs in fluid levels that hemodialysis brings.
But hemodialysis is easier on staff.