
- medications
- pharmacokinetics
- dosage calculations
- routes of administration
- e-CPS
- Dal Pharm Drug Info
- RxFiles
Section Links
Antihypertensives
There are four main classes of antihypertensives, as discussed below. While they are used to control blood pressure, different combinations are preferred in different conditions or diseases.
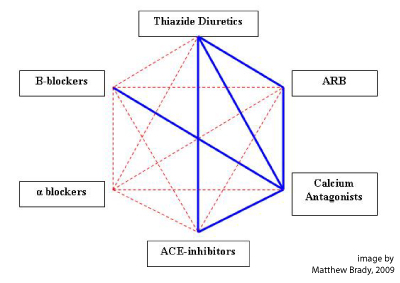 Combinations of blood pressure control medications is important for many patients to reach optimal pressure control.
Combinations of blood pressure control medications is important for many patients to reach optimal pressure control.
The image at left depicts suggested combinations to trial, with blue lines being good combinations and red lines less so.
- ACE inhibitors/ARBs
- beta blockers
- calcium channel blockers
- diuretics
ACE inhibitors and ARBS (Angiotensin II Receptor Blockers)
ACE inhibitors block the production of ANG II, reducing blood pressure. They also prevent inactivation of bradykinin by kininase, leading to increased vasodilation.
Not best for black people (low renin). Do not use in pregnant women.
Uses
- moderate to severe hypertension
- reduces proteinuria in diabetes mellitus, especially in combination of ACEi and ARB
- post-MI, preventing remodeling and hypertrophy
- heart failure
- chronic kidney disease, acting to reduce intraglomerular pressure
Drug
sACE-Inhibitors |
Absorption Affected by Food |
Strengths (mg) |
Regular Recommended Starting Dose (monotherapy) |
Target Dose |
Perindopril |
No |
2, 4, 8 |
4 mg once daily |
4-8 mg daily |
Trandolapril |
No |
0.5, 1, 2, 4 |
1 mg once daily |
1-2 mg daily |
Quinapril |
No |
5, 10, 20, 40 |
10 mg once daily |
10-20 mg daily |
Fosinopril |
No |
10, 20 |
10 mg once daily |
20 mg daily |
Benazepril |
No |
5, 10, 20 |
10 mg once daily |
20 mg daily |
Captopril |
Yes |
12.5, 25, 50, 100 |
25 mg bid to tid |
50 mg b-tid |
Enalapril |
No |
2.5, 5, 10, 20 |
5 mg once daily |
10-40 mg single or 2 divided doses |
Ramipril |
No |
1.25, 2.5, 5, 10 |
2.5 mg once daily |
2.5-10 mg daily |
Cilazapril |
Yes |
1, 2.5, 5 |
2.5 mg once daily |
2.5-5 mg daily |
Lisinopril |
No |
5, 10, 20 |
20 mg once daily |
10-40 mg daily |
Table 2. Heart Failure
ACE- Inhibitor |
Target Dose |
Ramipril |
5 mg bid or 10 mg daily |
Perindopril |
4 mg daily |
Quinapril |
40 mg daily or 20 mg bid |
Captopril |
50 mg tid |
Cilazapril |
2.5 mg daily |
Enalapril |
10 mg bid |
Lisinopril |
20-35 mg daily |
All ACEIs have a duration of action approximately 24 hours except for captopril (6-12 hrs)
Adverse Drug Reactions
It is very important to recheck plasma creatinine and potassium 7-14 days after starting an ACE or ARB. An increase of 20% in sCR, a 20% fall in eGFR, or a rise in potassium above 5.5 mmol/L should prompt change in medication, further investigation, or potassium reduction diet.
- cough: the most common reason people stop
- hypotensiondecreased renal perfusion in volume depletion
- hyperkalemia due to reduced aldosterone production
- teratogenic
Mechanism of Action
Competitive inhibitor of ACE-I
Indirectly decreases aldosterone
Decreases TPR
Increased bradykinin levels
Decreases blood pressure, preload and afterload without changes in HR or norepinephrine rebound.
Can cause a significant regression in LFH
Increase in stroke volume and cardiac index as well as decreases in right atrial pressure, MAP, and systemic vascular resistance in those with CHF.
Increases renal perfusion via dilation of the efferent arteriol and decreases renal vascular resistance
Decreases proteinuria and stabilizes renal function (in chronic renal failure) regardless of the ability to decrease blood pressure.
- losartan

- medications
- pharmacokinetics
- dosage calculations
- routes of administration
- e-CPS
- Dal Pharm Drug Info
- RxFiles
Section Links
Antihypertensives
There are four main classes of antihypertensives, as discussed below. While they are used to control blood pressure, different combinations are preferred in different conditions or diseases.
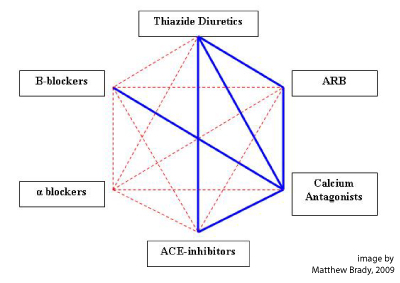 Combinations of blood pressure control medications is important for many patients to reach optimal pressure control.
Combinations of blood pressure control medications is important for many patients to reach optimal pressure control.
The image at left depicts suggested combinations to trial, with blue lines being good combinations and red lines less so.
- ACE inhibitors/ARBs
- beta blockers
- calcium channel blockers
- diuretics
ACE inhibitors and ARBS (Angiotensin II Receptor Blockers)
ACE inhibitors block the production of ANG II, reducing blood pressure. They also prevent inactivation of bradykinin by kininase, leading to increased vasodilation.
Not best for black people (low renin). Do not use in pregnant women.
Uses
- moderate to severe hypertension
- reduces proteinuria in diabetes mellitus, especially in combination of ACEi and ARB
- post-MI, preventing remodeling and hypertrophy
- heart failure
- chronic kidney disease, acting to reduce intraglomerular pressure
Drug
sACE-Inhibitors |
Absorption Affected by Food |
Strengths (mg) |
Regular Recommended Starting Dose (monotherapy) |
Target Dose |
Perindopril |
No |
2, 4, 8 |
4 mg once daily |
4-8 mg daily |
Trandolapril |
No |
0.5, 1, 2, 4 |
1 mg once daily |
1-2 mg daily |
Quinapril |
No |
5, 10, 20, 40 |
10 mg once daily |
10-20 mg daily |
Fosinopril |
No |
10, 20 |
10 mg once daily |
20 mg daily |
Benazepril |
No |
5, 10, 20 |
10 mg once daily |
20 mg daily |
Captopril |
Yes |
12.5, 25, 50, 100 |
25 mg bid to tid |
50 mg b-tid |
Enalapril |
No |
2.5, 5, 10, 20 |
5 mg once daily |
10-40 mg single or 2 divided doses |
Ramipril |
No |
1.25, 2.5, 5, 10 |
2.5 mg once daily |
2.5-10 mg daily |
Cilazapril |
Yes |
1, 2.5, 5 |
2.5 mg once daily |
2.5-5 mg daily |
Lisinopril |
No |
5, 10, 20 |
20 mg once daily |
10-40 mg daily |
Table 2. Heart Failure
ACE- Inhibitor |
Target Dose |
Ramipril |
5 mg bid or 10 mg daily |
Perindopril |
4 mg daily |
Quinapril |
40 mg daily or 20 mg bid |
Captopril |
50 mg tid |
Cilazapril |
2.5 mg daily |
Enalapril |
10 mg bid |
Lisinopril |
20-35 mg daily |
All ACEIs have a duration of action approximately 24 hours except for captopril (6-12 hrs)
Adverse Drug Reactions
It is very important to recheck plasma creatinine and potassium 7-14 days after starting an ACE or ARB. An increase of 20% in sCR, a 20% fall in eGFR, or a rise in potassium above 5.5 mmol/L should prompt change in medication, further investigation, or potassium reduction diet.
- cough: the most common reason people stop
- hypotensiondecreased renal perfusion in volume depletion
- hyperkalemia due to reduced aldosterone production
- teratogenic
Mechanism of Action
Competitive inhibitor of ACE-I
Indirectly decreases aldosterone
Decreases TPR
Increased bradykinin levels
Decreases blood pressure, preload and afterload without changes in HR or norepinephrine rebound.
Can cause a significant regression in LFH
Increase in stroke volume and cardiac index as well as decreases in right atrial pressure, MAP, and systemic vascular resistance in those with CHF.
Increases renal perfusion via dilation of the efferent arteriol and decreases renal vascular resistance
Decreases proteinuria and stabilizes renal function (in chronic renal failure) regardless of the ability to decrease blood pressure.
- losartan
Adverse Drug Reactions
Decrease in aldosterone causes potassium retention in most patients.
Angioedema has been reported with use of some ACEIs.
Oliguria, azotemia, and renal failure can occur in those with severe HF.
Severe hypotension can occur with those already hypovolemic or treated with other antihypertensives.
Dry cough is a common side effect.
Taste disturbance common with captopril.
Contra-indications and Drug Interactions
Renal arterial stenosis.
Use of ACEIs in pregnancy has been associated with fetal abnormalities.
ACEI + Spironolactone can cause life threatening hyperkalemia and should not be initiated unless under very close observation.
NSAIDS can antagonize the antihypertensive effects of ACEI.
ACEI + Lithium can cause lithium toxicity
Pharmacokinetics, metabolism and excretion
All have active metabolites except for captopril and lisinopril.
Most all ACEIs are excreted solely by the kidney but both renal and fecal elimination is seen with: Benazepril, fosinopril, quinapril, ramipril, and trandolapril.
Advice for Clinical Practice
Adjust dose 2-4 weeks after initiating ACEI if inadequate response and always ask about use of NSAIDS as this can contribute to treatment resistant hypertension.
Advise to discontinue ACEI if swelling of the face or lips occur. If swelling of tongue and/or throat occurs then administration of epinephrine is required.
It is very important to recheck plasma creatinine and potassium 7-14 days after starting an ACE or ARB. An increase of 20% in sCR, a 20% fall in eGFR, or a rise in potassium above 5.5 mmol/L should prompt change in medication, further investigation, or potassium reduction diet.
-
cough: the most common reason people stop
-
hypotension decreased renal perfusion in volume depletion
-
hyperkalemia due to reduced aldosterone production
-
teratogenic
If dry cough occurs and is particularly bothersome then re-challenging with another ACEI is appropriate. Cough usually subsides within 1-3 weeks but may take up to 3 months. Switching to an ARB may be necessary.
ACEI should be a priority for patients with HF or post-MI since they are shown to have a mortality benefit.
When adding an ACEI to a patient already on a diuretic it is suggested to with hold the diuretic 2-3 days prior to initiating the ACEI.
The combination of ACEI + ARB should be avoided unless patients with compelling indications like those with CHF.
ACEI’s should be strongly considered in those with diabetes with or without proteinuria due to their beneficial effects on GFR.
Warn patients that ‘no-salt’ or ‘half-salt’ substitutes might not be appropriate because they’re mostly potassium salts.
Beta Bockers
Do not start in people over 60.
Drugs that inhibit the sympathetic nervous system are often used in the treatment of cardiovascular disease
Uses
- moderate to severe hypertension
- angina
- congestive heart failure
- acute coronary syndromes, though no real evidence of improving outcomes
Classes
Centrally acting
- act on the BP control centre in the brain
- thought that they act on α2 receptors to inhibit NE release
- side effects include sedation
- methyldopa
- clonidine
Beta-blockers
- decrease cardiac output (both HR and contractility)
- also decrease renin release, leading to lowered Na, water retention and vasodilation
- can be used (off-label) for stage fright
- makes exercise difficult
- propanolol: β1 and β2 antagonist
- metoprolol: β1 antagonist
- atenolol
- acebutamol
- bisoprolol
Alpha-blockers
- block α1 receptors on vascular smooth muscle cells, increasing vasodilation
- parazosin
Mechanism
- competitively inhibits beta1 receptors reducing HR, contractility, BP, and MVO2
- increases duration of diastole
- beta blockers work against renin.
Dose and Half Life
oral therapy sufficient in most case of ACS, though IV metoprolol can also be done 5mgx3 over 15 min
Adverse Drug Reactions
increasing doses of beta blockers causes loss of cardioselectivity and
can substantially risk of stroke or diabetes
short term
- avoid acute adminstration in unstable patients with hypotension or overt HF
- bradycardia and heart block
- bronchospasm
- peripheral vasoconstricion
- fatigue, lethargy
long term
- depression, vivid dreams, nightmares
Counter-Indications and Drug Interactions
do NOT combine with NDHP CCBs, as this can cause bradycardia
- absolute: asthma
relative:
- tendency to bronchospasm
- insulin dependent T2DM
- conduction system disease
- peripheral vascular disease
Calcium Channel Blockers
Diuretics
Diuretics act to promote sodium and water loss. They are used to treat hypertension (especially thiazides), heart failure, cirrhosis, nephrotic syndrome, and other causes of edema.
Loop Diuretics
Loop diuretics are powerful drugs that inhibit the Na/K/2Cl triporter in the thick ascending limb, possibly be competing with chloride. This drop in Na and K resorption leads to diuresis and kaluresis.
A loss of renal concentrating and diluting capacity leads to impaired preservation of water and electrolytes during periods of dehydration.
Hypokalemia, hypomagnesemia, and occasionally hyponatremia can be due to loop diuretic use. Furosemide (Lasix) is the most common loop diuretic. Perhaps alkalosis too due to hypokalemia?
Not good for HTN, as it needs to be dosed TID. Good if Cr >130 mmol
Thiazides
Thiazides are key drugs in treating hypertension. They inhibit NaCl transport into the distal convoluted tubule, preserving loop function.
These can also produce hypokalemia.
Hyponatremia is fairly common as volume contraction engages ADH and much free water is reabsorbed. Electrolytes need to be monitored after beginning therapy.
Potassium-Sparing Diuretics
These drugs antagonize the effects of aldosterone at the cortical collecting tubule and late distal tubule.
Spironolactone inhibits the aldosterone receptor, while triamterene and amiloride appear to inhibit Na flux through ion channels in the lumenal membrane.
Hyperkalemia can result due to decreased K secretion.
Other
Acetazoamide acts on the proximal tubule